© Borgis - New Medicine 4/2013, s. 126-128
Jolanta Jadczyszyn, *Lidia Zawadzka-Głos, Małgorzata Dębska
Meningitis and encephalitis of the etiology of Streptococcus pneumoniae – a case report
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Summary
Meningitis occurs with infiltration of a soft and a spider as a result of penetration of bacteria into the fluid of the temporal bone. Most often caused by Haemophilus influenzae type b (Hib) and Streptococcus pneumoniae. In children, acute otitis media is four times more common cause of intracranial and infratemporal complications than chronic inflammation. Predominant intracranial complications in children is meningitis. The diagnosis is based on an examination of cerebrospinal fluid. The treatment consists of removal of the focus of purulent otitis media and intensive antibiotic therapy.
INTRODUCTION
Intracranial complications involve children and young people more often than adults (1, 2). They mainly occur in the course of acute otitis media, rarely -in chronic otitis media with cholosteatoma or granulation tissue (1, 3). The most common complication is meningitis (2, 4, 5). The characteristic symptoms of meningitis and encephalitis are: persistent fever (including septic fever), headache, nausea and vomiting, confusion, agitation, seizures and meningeal signs (neck stiffness, positive Brudzinski sign). The predominant pathogens are the most common intracranial complications pneumococcus, Pseudomonas, sticks G (-), rarely stick G (+) and fungus (1, 4). The infection spreads to the interior of the skull directly to the inflamed bone, its natural or traumatic loss, by veins or anatomical connections with ear structures and skull structures. The course of complications depends on a patient’s immune response, coexisting diseases, treatment, pathogenic bacteria and their sensitivity to antibiotics.
CASE REPORT
A 4-year-old boy was admitted to Children’s Hospital in Warsaw with severe conditions. 6:45 because of the seizure of the short-term loss of consciousness with associated vomiting, which occurred at night. A 3-day Medical history: fever to 40°C, headache, and catharal otitis media left, the patient isn’t treated with an antibiotic. In the case the patient suffered from otitis several times. Last otitis media treated with antibiotics a month ago. In addition, this history is without any strains When examined, the patient conscious, pale skin with features of dehydration, stiff neck, eyes flat, narrow lazily react to light, exotropia. Lung and heart auscultation was normal. Efficient respiratory and circulatory. BP 115/80 mmHg, HR 100 bpm, breaths 30/min, saturation of 100% without oxygen, TPR 38.6°C. In laboratory studies increased markers of inflammation and D-dimers (tab. 1).
Table 1. Laboratory tests.
| Tests | 1 day | 3-4 day |
| WBC (4.5-13 thous.) | 31.7 | 13.8 |
| RBC (4.3-5.5 mln) | 4.47 | 2.92 |
| HB (10.9-14.2 g/dl) | 12.7 | 8.3 |
| HCT (34-41%) | 38.4 | 25.6 |
| PLT (250-550 thous.) | 259 | 213 |
| Lymph % | 1.9 | 6.7 |
| Neut % | 97.8 | 86.5 |
| Mono % | 0.3 | 6.4 |
| INR (0.9-1.25) | 1.6 | 1.43 |
| APTT (26-36 sec.) | 29.07 | 44.26 |
| D-dimery (170-550 ug/L) | 3127 | 3039 |
| CRP (0-1 mg/dl) | 22.2 | 29.1 |
| Fibrynogen (2-4 g/l) | 8.03 | 11.31 |
| AST (15-40 U/L) | 17 | 105 |
| ALT (10-35 U/L) | 16 | 33 |
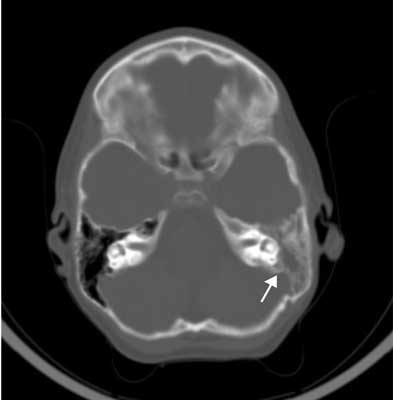
Taken blood culture and cerebrospinal fluid before turning on intravenous antibiotics (Vancomycin and Biotaksym). About hrs. 9:08 made head CT with contrast. It was airless mastoid cells, and cells of the tympanic cavity top of the pyramid of the temporal bone on the left side, segmental breaking the continuity of lamina inner the mastoid process around the left sigmoid sinus. Brain tissue without change (fig. 1).
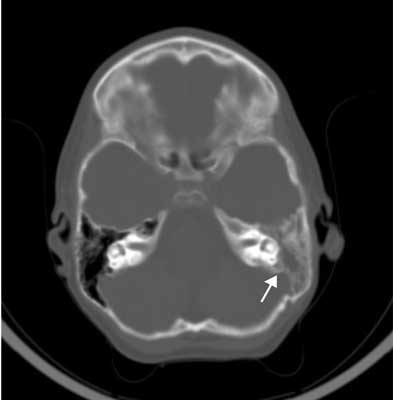
Fig. 1. Mastoiditis on the left side.
Because of the severe condition of the patient and the lack of anesthesiological consent for general anesthesia on the day of admission, bilateral paracentesis. Obtained material is sent for microbiological examination. Over the next few days of hospitalization were observed purulent leakage from the left ear. Within four hours of hospitalization (at approx. 10:40) the patient’s condition deteriorated. Intensified disturbances of consciousness and seizures, the boy anxious, agitated, stiff neck from unbent body position, eyes widened. There were breathing problems. After the anesthesiological consultation, the patient was transferred to the Intensive Care Unit and was intubated. Observed characteristics of highintracranial pressure with very high blood pressure and BP 180/130 mmHg, with an accompanying bradycardia, impaired peripheral perfusion. It has been found a high degree of centralization of the blood circulation. Drugs for the treatment included decongestants. The two day hospital stay after learning the symptoms of intracranial hypertension, and clotting disorders equalized again lumbar puncture was performed, which confirmed the diagnosis of maningitis (tab. 2). The inoculation of bacteria not cultured fluid. However, in the inoculation of blood showed etiology Streptococcus pneumoniae. In many cultures produced they were found to colonize a large bacterial flora (tab. 3).
Table 2. Testof cerebrospinal fluid.
| Color | Drab |
| Clarity | Cloud |
| Pleocytosis (0-5/ul) | 8400/ul |
| Reaction Noone-Appelta | +++ |
| Reaction Pandy’ego | +++ |
| Total protein (15-45 mg/dl) | 374 mg/dl |
| Glucose (40-70 mg/dl) | 66 mg/dl |
Table 3. Test bacteriological.
| Blood culture | Streptococcus pneumoniae |
| Cerebrospinal fluid | Negative |
| The left ear swab | Negative |
| The right ear swab | Bacillus spp. |
| Urine culture | Negative |
| Throat swab | Staphylococcus spp.
Koagulazo (-) numerous |
| Secretions from the respiratory tract | Morganella morganii,Enterobacter cancerogenus |
| Recital swab | E. coli, Morganella morganii, Staphylococcus spp. |
Surgical treatment (in the 2nd day) consisted of making a wide left-hand antromastoidectomia. Granulation tissue filling the mastoid cells were sent for histopathological examination. In the area of the sigmoid sinus, a fistula bone and a pus were found, in the aditus ad the antrum of a granulation tissue that was removed.
After three days of hospitalization the boy still with severe condition. An incident occured again: symptoms of increased intracranial pressure, i.e. dilated pupils, anizokoria OL 3 mm > OP 2 mm, shaking his left hand and symptoms of cardiovascular, three points on the Glasgow scale. Control head CT was performed (fig. 2). It was a large diffuse swelling of the brain, base of the brain vessels and fluid spaces tight, light chambers III and IV invisible, visible areas of different density. In this study, there was no resistance index and angioCT venous sinus thrombosis (fig. 3).

Fig. 2. Edema of the brain.

Fig. 3. AngioCT was normal.
Neurological consultation stated: hemiparesis on the right, swelling of the brain (without impaction) in the course of the meningitis, pupils quite narrow, even, do not respond to light. Abnormal EEG, low voltage. The head CT examinations were gradual resolution of edema. Because of slight improvement in the patient’s condition, a permanent mechanical ventilation, breathing CMV ventilator breaths own suppressed, poor neurological status and lack of saliva swallowing after tracheostomy in 20 day of hospitalization and percutaneous gastrostomy (PEG) at the age of 38. During hospitalization, intensive antibiotic used 20 nights: Biotaksym, vancomycin, diflukan, then 9 nights: augmentin and 30 nights without antibiotic treatment. The patient’s condition improved. The boy begins to respond to pain and touch, he opens his eyes, convulsions subsided, there were breathing their own 28/min. Ultrasound examination of the vocal folds of the larynx mobility symmetrical correct. Exchanged tracheostomy tube to tube phoniatric at age 47, and then performed removal of the tube (52 day). The oy with hemiparesis on the right, with a history of sepsis and meningitis, spinal transferred to the pediatric unit, and then qualified for rehabilitation.
CONCLUSIONS
Intracranial complications occur in 0.5-4% of all otitis media (6). Now the most common intracranial complication in children is meningitis (2-4). Especially exposed to meningitis in the course of otitis are children with congenital middle ear and facial defects. Frequent pathological connection between the middle ear and the middle and back of the skull cavity can be stated (7). The meningitis and encephalitis may occur as inflammation of the serum with a good prognosis, which persists after the operation ear, and turn antibiotic. Primary serous inflammation of tires in young children is a consequence of stopping pus in the tympanic cavities and occurs at the beginning of otitis (8). However, bacterial meningitis often the etiology of Streptococcus pneumoniae are the main cause of neurological complications (5). In patients with suspected inflammation of meningitis always perform the test cerebrospinal fluid, which is the only criterion for distinguishing. You should also perform imaging studies of temporal bone CT, which allows the assessment of the severity of inflammatory ear and concomitant bone destruction. Treatment consists of removal of the focus of purulent otitis media and intensive intravenous antibiotic therapy-III generation cephalosporin with vancomycin. The treatment can also consider giving rifampicin or meropenem (5, 6). The treatment regimen is a consequence of the increasing prevalence of bacteria resistant to penicillins and cephalosporins I and II generation (5, 6, 9). Now intracranial complications are stilla difficult diagnostic and therapeutic problem because of non-specyfic symptoms associated with common antibiotics. Widely used antibiotics can cause inflammation in the transition state of subacute and latency of infection. Complications may occur more frequently with increasing resistance to antibiotics and the growing number of immunocompromised patients. The prognosis of intracranial complications is still significant, and the mortality rate amounts 5-15% (6, 10).
Piśmiennictwo
1. Otolaryngologia dziecięca, red. M. Chmielik, PZWL; Warszawa 2006. 2. Samuel J, Fernandes CMC, Steinberg JL: Intracranial otogenic complications: a persisting problem. The Laryngoscope 1986, 96; 3: 272-278. 3. Skotnicka B: Complications of otitis media in children in the era of antybioticotherapy. Otolaryngol Pol 2007; 61(5): 779-783. 4. Kangsanarak J, Navacharoen N, Fooanant S, Ruckphaopunt K: Intracranial Complications of Suppurative Otitis Media: 13 Years’ Experience. American Journal of Otology; 1995: 104-109. 5. Migirov L, Duvdevani S, Kronenberg J: Otogenic intracranial complications: a review of 28 cases. Acta Otolaryngol 2005; 125(8): 819-822. 6. Ciorba A, Berto A, Borgonzoni M, Grasso DL et al.: Pneumocephalus and meningitis as a complication of acute otitis media: case report. Acta OtorhinolaryngolItal 2007; 27(2): 87-89. 7. Otolaryngologia dziecięca, red. D. Gryczyńska, Alfa-Medica Press; Bielsko-Biała 2007. 8. Otolaryngologia kliniczna, red. A. Zakrzewski, PZWL; Warszawa 1981. 9. Damergis JA, Chee K, Amitai A: Otogenic pneumococcal meningitis with pneumocephalus. Emerg Med 2010; 39(3): 109-112. 10. Janczewski G: Otolaryngologia praktyczna, Via Medica; Gdańsk 2005.