© Borgis - Postępy Nauk Medycznych 7/2009, s. 539-544
Maciej Michalik1, *Edward Stanowski2
Outcome of surgical treatment of morbid obesity
Wyniki leczenia operacyjnego otyłości olbrzymiej
1Department of General and Vascular Surgery; F. Ceynowa Specialist Hospital, Wejherowo, Poland
Head of Department: Maciej Michalik, MD
2Department of General, Oncological and Thoracic Surgery, Military Institute of Medicine, Warsaw, Poland
Head of Department: Krzysztof Pa?nik, MD, PhD
Streszczenie
utcome of morbid surgical obesity treatment. The authors describe the outcome of surgical treatment of morbid obesity depending on the type of the procedure, patients´ preoperative BMI, age and sex. The analysis includes weight loss, resolution of co-morbidities, quality of life, morbidity and mortality. Mortality was compared between patients treated surgically and conservatively. Attention was paid to the correlation between the surgeon´s experience and the outcome of the treatment.
Summary
Przedstawiono wyniki chirurgicznego leczenia otyłości w zależności od rodzaju wykonanej operacji, wskaźnika BMI, wieku i płci operowanych. Analizowano ubytek masy ciała, ustępowanie chorób towarzyszących, powikłania, śmiertelność, jakość życia. Porównano śmiertelność operowanych z osobami otyłymi nieleczonymi operacyjnie. Zwrócono uwagę na związek liczby operacji wykonanych przez chirurga i w danym ośrodku na wyniki.

Obesity can be treated conservatively (diet, medications, physical activity) or surgically. Lack of permanent outcome of the conservative treatment is presented in figure 1 (1).
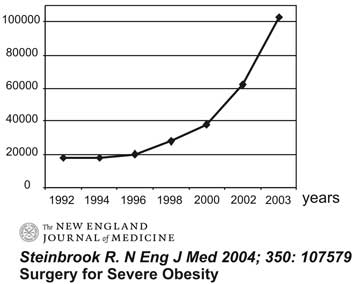
Fig. 1. Obesity conservative treatment outcome.
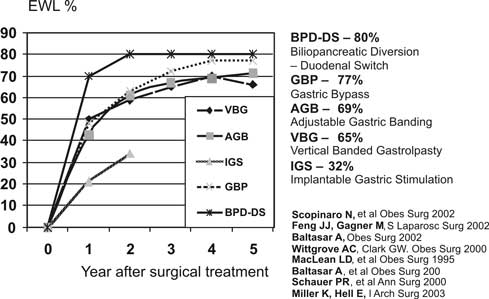
Such discouragingly poor results of the conservative treatment of obesity resulted in the development of surgical techniques in the second half of the 20th century. An increase in the number of surgically treated obesity cases in the US confirms this fact. Figure 2 shows how much the number of surgical procedures in the US has increased recently (2).
Fig. 2. Number of US surgical procedures for obesity treatment.
Of note is the fact that in 2006 the number of surgical procedures for obesity treatment in the US exceeded 171,000 and was higher than the number of cholecystectomies.
What do we expect from the surgical treatment of obesity? The surgical treatment can be acceptable if it meets the following conditions:
It will result in a considerable and permanent decrease in body mass (60-80% of overweight);
It will make co-morbidities regress or alleviate them substantially;
It will affect the quality of life including the possibility to go back to work;
The perioperative complication and mortality rates will be acceptable.
Body mass loss following the surgical treatment of obesity
One of the objectives of surgical obesity treatment is body mass loss. The treatment is considered effective if at least 50% excess weight loss (EWL) is achieved. Following different types of surgery, this parameter varies; it is also more or less permanent. Mean EWL at 12 months after laparoscopic procedures is for DS-BPD 70-80%, for G-B 77%, for AGB 69% (3, 4). These data prove that the most extensive procedures, i.e. with potentially the highest risk for complications, result in the highest body mass loss (fig. 3).

Fig. 3. Excessive Weight Loss – EWL.
Yet, many studies also report that such surgery causes the biggest metabolic disturbances in the form of deficiency syndromes. A patient after surgical obesity treatment loses weight. But is this weight loss permanent? Or sufficiently long? Today, when the follow-ups have been long enough, we can say it is. Patients with a low-pressure adjustable gastric band lose weight regardless of their BMI before surgery (from 35 to more than 60 kg/m2), age or sex, and the corrected body mass is maintained for many years with only minor modifications at 12 months after surgery (5).
When qualifying a patient for an appropriate type of surgery the parameters which must be considered are: the past highest and present body mass, co-morbidities, and the patient´s compliance in each stage of treatment. This should make the surgical procedure bring expected and permanent results with the smallest risk for the patient.
Does the type of surgery affect the weight loss in the postoperative period? Many authors believe that the type and outcome of surgery cannot be associated with the body mass loss expressed in EWL.
The analysis of the type of surgery performed (weight loss has been reported in literature) shows that what Scopinaro introduced in 1976, i.e. biliopancreatic diversion (BPD) and duodenal switch (DS), lead to the greatest excess weight loss, in the range 65-75%, which is permanent. The fact has been confirmed by studies performed by Hess and Hess, Marceu et al. and many others (acc. 6,7). After reviewing the relevant world literature.
Neugebauer et al. designed guidelines for treating obesity for EAES and published them in 2007 (7). In the study mentioned above, the authors reported the following results. In the comparison of RYGN with VBG, a randomized trial carried out by Sugerman showed that EWL was higher after RYGB (68% vs 43%) but absorption disorders, vomiting and gastroenterostomy stenosis were more common after RYGB. These facts were confirmed by the studies performed by Hal et al., Howard et al., and Mac Lean et al. Randomized studies carried out by Nussel et al., which compared VBG with ASGB in open surgery with LASGB done by Morino et al., revealed that at 5 years EWL was similar in all patients. Rabkin et al. and Murr et al. compared BPD with RYGB and reported EWL to have dropped more after BPD (78 and 74%) than after RYGB (71 and 57%). Yet in a trial by Deveney et al., EWL decrease was similar in both groups. Bjardi et al. found EWL to have dropped more after LRYGB in comparison with LASGB – 64% vs 48%. Miller and Hell reported that at 12 months after laparoscopic surgery, EWL drop for DS-BPD was 70-80%, for LRYGB 77%, and for LASGB 69% (acc 6,7).
Pa?nik assessed EWL rate after restrictive surgery and found the highest weight loss after vertical banded gastroplasty (67%), smaller after LASGB (57%). Overall, 84% of his outcomes were good; a better outcome was observed in patients with BMI<50 (8).
Kwiatkowski assessed EWL rate at 12 months after various types of surgery and reported the weight loss as 77.5% after VBG and 60.8% after LASGB. A detailed analysis of the groups studied showed that after LASGB almost 20% failed to reach a 50% EWL, whereas in the VBG group, it was 5%, and in the LRYGB group, all patients exceeded 50% EWL (9).
A literature analysis proves that the highest body mass loss can be achieved after procedures in the following descending sequence: BPD-DS, RYGB, VBG, SG; after ASGB the weight loss is the smallest. The procedures which result in the biggest weight loss are the most difficult technically, need a long learning curve and are associated with the highest risk for such complications as bleeding and leakage as well as deficiency syndromes (vitamin deficiency, especially vitamin B, and microelements). The deficiency resulting from restrictive surgery is easy to supplement if patients are routinely monitored and supplemented accordingly. Such procedures as BPD-DS, RYGB and SG require more staple magazines and that makes them less cost-effective (acc. 6, 7).
The influence of the surgical obesity treatment on co-morbidities
Co-morbidities caused by obesity or accompanied by it include type 2 diabetes, arterial hypertension, coronary artery disease, lipid metabolism disorders, diseases caused by osteoarticular system overload, young women´s infertility, and others. Long studies on large groups of patients have proved that, in comparison to people with normal parameters, high BMI, waist circumference and body fat tissue percentage significantly influence the development of co-morbidities.
An important aspect of surgical obesity treatment is the resolution of co-morbidities. Following surgery, type 2 diabetes was found to subside in 74%, arterial hypertension in 57%, manifestations of gastroesophageal reflux in 55%, dyslipidaemia in 38%; EWL at 6 months was 30%, at 12 months 41%, and at 24 months 41%. Many studies do not show any difference or prove the differences insignificant in terms of resolution of co-morbidities depending on the type of surgery (7, 8, 9). Clegg et al. found diabetes to subside in 74% of patients, hypertension in 57%, manifestations of gastroesophageal reflux in 55%, dyslipidaemia in 38% (10). According to Kwiatkowski, Brolin et al. found that co-morbidities subsided or improved in 95% of patients who had undergone surgical obesity treatment. Gordon and Kannel reported NT, dyslipidaemia and carbohydrate disturbances resolution in over 50%, and significant improvement in 24% at 12 months following surgery. Three years after bariatric surgery (VBG, LASGB), Hell and Miller found that co-morbidities had improved or resolved completely in more than 80% of surgical patients. Alvarez et al. found that arterial hypertension had subsided in 90% of patients, and 60% of them could discontinue hypoglycaemic therapy (acc. 6, 7, 8, 9).
In Polish studies, Pa?nik compared the outcome of vertical banded gastroplasty and adjustable gastric band restrictive surgery procedures and found diabetes to have subsided in 28% and improved in a further 44%. Arterial hypertension was found to have subsided in 31% and improved in 44% of patients. He found no significant relevant differences between the types of surgery (8).
Kwiatkowski (9) analyzed metabolic syndrome (MS) improvement after various bariatric surgical procedures and found that MS subsided in 44.5% of patients with BMI below 50; in those with BMI above 50, it subsided in 79.4%. A similar beneficial phenomenon is observed over patients´ age.
Although MS subsided in 50% of patients aged below 50 years, it subsided in 72% of those older than 50. One year after surgical obesity treatment procedures, the metabolic syndrome prevalence decreased from 53% to below 16%. When types of surgery were analyzed, LRYGB was found to decrease MS in 67.2%, LASGB in 54.6% and VGB in 63%. Arterial hypertension decreased from 54.6% to 16.4% at 12 months after surgery. When the type of surgery and persistent hypertension were analyzed, hypertension was present in 7.5% of patients after LASGB, 20% after VGB and 26% after LRYGB. MS subsided in 63-75% regardless of the type of surgery but in the case of arterial hypertension, the most effective was the simplest procedure, i.e. LASGB, and the least effective was LRYGB. Following surgery, diabetes improved from 39.5% to 21.7%. Glycaemia subsidence, depending on the type of surgery, was 39% after VBG, 50% after LRYFB, 66.7.5 after LASGB. Hypertriglyceridaemia before surgery was diagnosed in 39.5% and at 12 months after surgery in 13.5%, so it subsided in 65% of patients who underwent surgery. The best outcome at 12 months after surgery was observed after VBG (71.9%), after LRYGB (64.3%), and after LASGB (56.2%). HDL cholesterol fraction was lowered in 40% of obese patients before surgery, and in only 8.5% at 12 months after surgery. The best outcome was achieved in the LRYGB group (88.9%), in the VGB group (80%), and in the LASGB group (66.7%). MS prevalence analysis proved to be BMI dependent. In patients with BMI<50, MS improved: after LASGB from 26.5% to 2.0%, after VBG from 56.7% to 13.3%; after LRYGB an improvement was observed in all surgical patients. In the excessive obesity group, with BMI>50, MS improved in the LASGB group from 75% to 25%, in the VGB group from 70% to 50%, and in the LRYGB group from 86.6% to 26.7%. When MS prevalence was analyzed in terms of surgery type, patients´ age and sex, no relations between MS improvement and these parameters were found (9).
How surgical obesity treatment affects the quality of life
When obesity treatment outcome is assessed, the assessment should include body mass loss, improvement in co-morbidities but also changes in the quality of life. The outcome is greatly influenced by surgery-induced complications (both short- and long-term) and, first of all, perioperative mortality (complications resulting from surgical obesity treatment are discussed in another paper). Just as important is the aesthetic effect of body mass reduction in the form of excessive skin, post-operative scars and others (10, 11). The results that are reported by physicians treating obesity conservatively and those published from surgical trials are very discrepant. They highlight perioperative mortality and surgery-related complications. Simultaneously, they reveal a completely different approach to the surgical treatment of obesity. This particularly concerns the choice of the moment a surgical procedure should be carried out. Unfortunately, physicians still commonly believe that the surgical procedure is an extreme. Surgeons argue that the surgical procedure should be undertaken when two attempts of comprehensive conservative treatment have failed or when BMI exceeds 40 because such patients will not succeed in achieving a permanent result using conservative methods only (12).
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
24 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
59 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
119 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 28 zł
Piśmiennictwo
1. Miller K: I Konferencja „Zaawansowane Operacje Laparoskopowe”, Wejherowo-Gdynia, kwiecień, 2005.
2. Steinbrook R: Surgery for Severe Obesity. N Engl J Med 2004; 350, 1075-79.
3. Robrecht HGG: Van Hee-Biliopancreatic Diversion in the Surgical Treatment of Morbid Obesity. World J Surg 2004; 28, 435-444.
4. Miller K, Hell E: Laparoscopic surgical concepts of Morbid Obesity. Langebecks Arch Surg 2003; 388, 375-384.
5. Edwards M. A et al.: Benchmarking hospital outcomes for t, M. Sidhu, P. Royle,A. Walker-Clinical and cost effectiveness of surgery for morbid obesity: a systematic review and economic evaluation.- International Journal of Obesity 2003; 27,1167-1177.
6. Stanowski E, Paśnik K: Chirurgiczne leczenie otyłości – aktualny stan wiedzy Wideochirurgia
7. Neugebauer AEH et al.: EAES Guidelines for Endoscopic Surgery. Berlin 2006.
8. Paśnik K: Wpływ chirurgicznych metod restrykcyjnych przewodu pokarmowego na jakość życia i choroby współistniejące u chorych z otyłością. Praca habilitacyjna WIM Warszawa 2004.
9. Kwiatkowski A: Wpływ operacji bariatrycznych na zespół metaboliczny u chorych z otyłością. Praca doktorska WIM Warszawa 2008.
10. CleggA, Colquit J: Laparoscopic adjustable gastric banding. Surg Endosc 2007; 21, 1950-1956.
11. Gordon T, Kanel WB: Obesity and cardiovascular disease the Framnigham study. Clin Endocrinol Metab 1976; 5, 367-375.
12. Tatoń J, Czech A, Berna M: Otyłość. Zespół metaboliczny. PZWL, Warszawa, 2007.
13 Gan SS, Talbot ML, Jorgensen JO: Efficacy of Surgery in the management of obesity-related T2 DM - ANZ J. Surg. 2007; 77, 958-962.
14. Pope GD et al.: Life Expectancy Benefits of Gastric Bypass Surgery. Surg. Innovations 2006; 13, 4.
15. Marsk R et al.: Antiobesity Surgery in Sweden from 1980 to 2005. A Population-Based Study With A Focus on Mortality – Ann of Surg 2008; 248, 5.
16. Parker M et al.: Predictors of outcome after obesity surgery in New York State from 1991 to 2003. Surg Endosc 2007; 21, 1482-1486.
17. Adams TD et al.: Long-term Mortality after Gastric Bypass Surgery. The New England J of Medicine 2007; 357, 8.
18. Tweddle E A, Woods S, Blamey S: Laparoscopic gastric banding: safe and modestly successful – ANZ J Surg 2004; 74, 191-194.
19. Angstadt J, Whipple O: Developing a New Bariatric Surgery Program – Presented during the Plenary Session at the Annual Scientific Meeting and Postgraduate Course Program, Southern Surgical Congress, Savannah, Georgia, 2007; 10-13.
20. Gonzalez R et al.: Does experience preclude leaks in laparoscopic gastric bypass? – Surg. Endosc.2006; 20, 1687-1692.
21. Esteban Varela J, Wilson SE, Nguyen NT: Outcomes of Bariatric Surgery in the Elderly – Presented at the 17th Conference of the Southern Chapter ACS Bacara Resort and Spa Santa Barbara, CA, January 2006; 20-22
22. Cohen L et al.: Laparoscopic revisional bariatric surgery. Myths and facts. Surg Endsoc. 2005; 19, 822-825.
23. Andrew ChG et al.: Early results after laparoscopic Roux-en-Y gastric bypass: effect of the learning curve. Can J Surg 2006; Vol 49, No 6.
24. Kim TH et al.: Early U.S. outcomes of laparoscopic gastric banding for morbid obesity – Surg Endosc 2006; 20, 202-209.
25. Anderson JM: Gastric Bypass surgery Experiences Huge Gains in Popularity Despite of Risks - J. of Controversial Medical Claims, 2008; Vol 15, No 4.
26. Deng JY, Lourke DJ: 100 Robotic-Assisted Laparoscopic Gastric Bypass at a Community Hospital – Presented at the 19th Annual Scientific Meeting of the Southern California Chapter of the ACS in Santa Barbara, CA, 2008; 18-20.