© Borgis - New Medicine 4/2014, s. 136-138
*Konrad Wroński1,2, Zbigniew Masłowski2, Leszek Frąckowiak1,3, Zbigniew Kozielec4
Chromophobe renal cell carcinoma – case report and review of literature
1Department of Oncology, Faculty of Medicine, University of Warmia and Mazury, Olsztyn, Poland
Head of Department: prof. Sergiusz Nawrocki, MD, PhD
2Department of Surgical Oncology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland
Head of Department: Andrzej Lachowski, MD
3Department of Gynecology and Gynecologic Oncology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland
Head of Department: Leszek Frąckowiak, MD, PhD
4Department of Pathomorphology, Hospital Ministry of Internal Affairs with Warmia and Mazury Oncology Centre, Olsztyn, Poland
Head of Department: Zbigniew Kozielec, MD, PhD
Summary
Chromophobe renal cell carcinoma comprises about 5% of the total cases of renal cell carcinoma. This neoplasm is diagnosed in 6th decade of life. The incidence of chromophobe renal cell carcinoma is similar in male and female population. Prognosis of this type of renal carcinoma is better than in other types. The authors of this article presented a case of a 60-year-old Caucasian woman who was admitted to the hospital because of right kidney tumor. The patient two years ago was treated due to melanoma of the back. Therefore, there was suspicion of melanoma metastasis to the right kidney. The author performed a literature review on chromophobe renal cell carcinoma diagnosis and treatment.
INTRODUCTION
Renal cell carcinoma is the most common neoplasm of the kidney (1, 2). This malignant neoplasm accounts about 2-3% of all cancers and in the most cases is diagnosed sporadic during imaging examinations such as ultrasonography and computer tomography (1-4). Chromophobe renal cell carcinoma comprises about 5% of the total cases of renal cell carcinoma (1, 2). This neoplasm is diagnosed in 6th decade of life (5, 6). The incidence of chromophobe renal cell carcinoma is similar in male and female population (1, 4, 6).
CASE REPORT
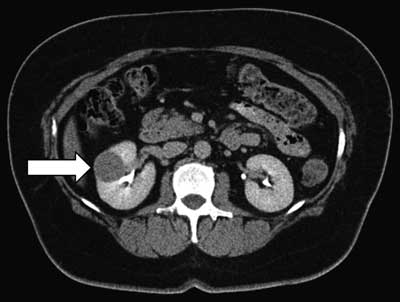
A 60-year-old Caucasian woman was referred to the Department of Surgical Oncology due to right kidney tumor which was incidentally examined in USG and CT scan (fig. 1). The size of this tumor in CT scan was 30 x 29 mm. The tumor was located in the middle of the right kidney cortex. In other organs of the abdomen and pelvic pathology has not been found in CT. In the interview, the patient reported no fever and pain. She had no any other symptoms, there was no history of weight loss and loss of appetite. The patient was treated for hypertension, ischemic heart disease and atherosclerosis. She had surgery two years ago due to melanoma of the back. There was no history of carcinoma in patient family.
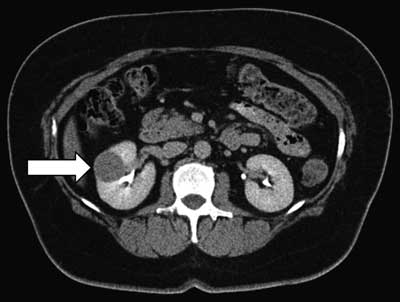
Figure 1. Tumor of the right kidney diameter 30 mm.
On physical examination the abdomen was soft, painless, without symptoms of peritoneal. The hemoglobin level was 131 g/l, the red blood cell count was 4.79x1012/l and other routine hematological examinations and biochemical tests were within normal limits.
Considering the tumor was located in the right kidney and there was suspicion of melanoma metastasis, an open right nephrectomy was performed (fig. 2, 3). During a surgical procedure, there was no bleeding. Patient after surgery felt good and did not complain of pain. The postoperative period was uncomplicated and the patient left the ward in the 7th day after surgery.

Figure 2. Macroscopic view of chromophobe renal cell carcinoma diameter 30 mm.

Figure 3. Chromophobe renal cell carcinoma is macroscopically mostly single, well-demarcated tumor, color gray to brown, to cross solid, without necrosis and blood hemorrhage.
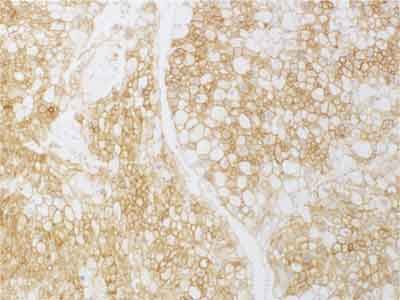
Pathological diagnosis was chromophobe renal cell caner (fig. 4, 5). Tumor cells were CK7 (+), CK20 (-), CD15 (-), vimentin (-), CD117 (+), Ki67 (+) in less than 1% of cells, EMA (+), Ep-CAM (+), E-cadherin (+) (fig. 6). Histopathologial advancement was: pT1a NX.
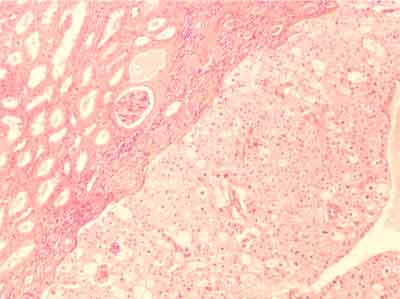
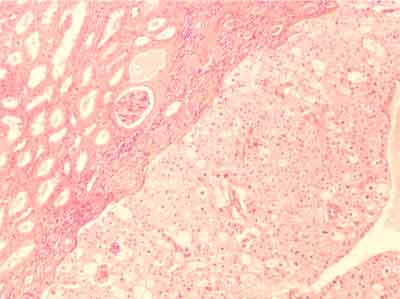
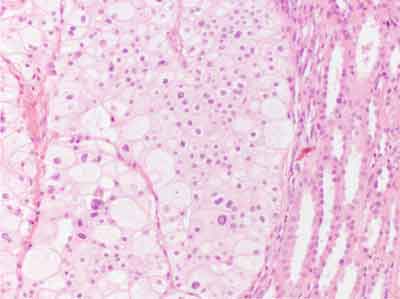
Figure 4. In microscopic image chromophobe renal cell carcinoma presents as a large, polygonal tumor cells with pale pink cytoplasm form a solid field separated by thin-walled blood vessels; staining with hematoxylin and eosin; 200 x.
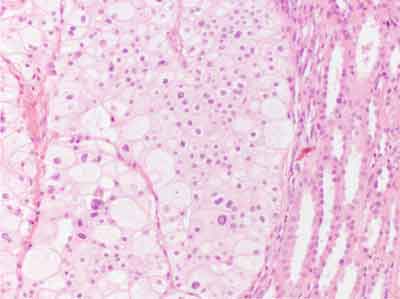
Figure 5. In microscopic image chromophobe renal cell carcinoma cytoplasm can be fine-or fine-grained with a clear around the nucleus; distinct cell membranes; staining with hematoxylin and eosin; 400 x.
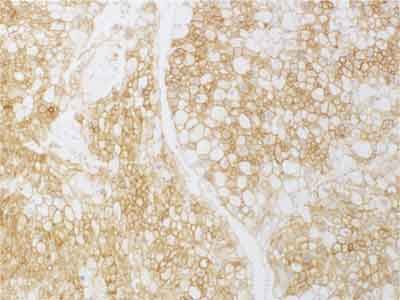
Figure 6. Tumor cells are positive to E-Cadherin.
The patient is now under the care of oncological outpatient at our hospital. After fourth months of surgery performed, there was no recurrence or metastasis.
DISCUSSION
Renal cell carcinoma is heterogeneous disease which is caused by different histological variants with a distinct clinical course and genetic changes (1-3). The categorization of renal cell carcinoma is based on the World Health Organization (WHO) classification (2, 4). The most common subtype of renal cell carcinoma is clear cell accounting 75%, papillary follows about 10%, chromophobe 5% and undifferentiated 10% of all cases (1-5).
Chromophobe renal cell carcinoma is diagnosed in 6th decade of life with the similar incidence in male and female population (1-5). Majority cases of this neoplasm are diagnosed in stage 1 and 2 (3, 5). Renal vein invasion is seen in up to 5% cases (3).
Clinical symptoms of chromophobe renal cell carcinoma are observed rarely. The triad of hematuria, pain and flank mass is present in a small percentage of patients (1-3). In advanced stadium of this neoplasm may be observed pyrexia, cachexia and weight loss (2-6).
The imaging technique for evaluation of renal masses is computer tomography. This techniques can differentiate the different subtypes of renal cell carcinoma. In CT scan inside chromophobe renal cell carcinoma there are observed calcifications up to 38% of cases (6,7).
First time chromophobe renal cell carcinoma was described in 1985 by Thoenes (7). Macroscopically this tumor present as a solitary, circumscribed and not capsulated mass (8). Microscopically this tumor contains large, polygonal cells with prominent cell membrane (9). This tumor cells have irregular nuclei with perinuclear clear halo (9-11).
Surgery is a fundamental treatment for chromophobe renal cell carcinoma. There is no standard of chemotherapeutic treatment for advanced chromophobe renal cell carcinoma (11-15). All information about chemotherapeutical treatment comes from retrospective and small prospective studies (12-14). In studies patients with advanced chromophobe renal cell carcinoma were treated mTOR inhibitors, c-Kit inhibitors and tyrosine kinase inhibitors (11-15).
A number of recent research, reported relatively good prognosis and survival rates for patients with chromophobe renal cell carcinoma. This good survival rates are caused by the detection of cancer disease at an early stage. Incidence of metastatic disease is observed up to 7% of cases (10). Metastases are observed in liver (39%) and lung (36%). Even in metastatic disease chromophobe renal cell carcinoma has better prognosis than papillary renal cell carcinoma. Median survival with metastases in chromophobe renal cell carcinoma is 29 months to 5.5 months in papillary renal cell carcinoma (11).
The treatment of renal cell carcinoma often need multimodal therapy so that it is important to treat such patients in high specialized oncological centers where treatment strategy for a patient is planned by several specialists.
Piśmiennictwo
1. Gndolo L, de la Taille A, Schips L et al.: Chromophobe renal cell carcinoma: comprehensive analysis of 104 cases from multicenter European database. Urology 2005; 65: 681-686. 2. Cheville JC, Loshe CM, Zincke H et al.: Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma. Am J Surg Pathol 2003; 27: 612-624. 3. Capitanio U, Cloutier V, Zini L et al.: A critical assessment of the prognostic value of clear cell, papillary and chromophobe histological subtypes In renal cell carcinoma: a population-based study. BJU Int 2009; 103: 1496-1500. 4. Crotty TB, Farrow GM, Lieber MM.: Chromophobe cell renal carcinoma: clinicopathological features of 50 cases. J Urol 1995; 154: 964-967. 5. Lee WK, Byun SS, Kim HH et al.: Characteristics and prognosis of chromophobe non-metastatic renal cell carcinoma: a multicenter study. Int J Urol 2010; 17: 898-904. 6. Amin MB, Paner GP, Alvarado-Cabrero I et al.: Chromophobe renal cell carcinoma: histomorphologic characteristics and evaluation of conventional pathologic prognostic parameters in 145 cases. Am J Surg Pathol 2008; 32: 1822-1934. 7. Thoenes W, Storkel S, Rumpelt MJ.: Human chromophobe cell renal carcinoma. Virchows Arch Cell Pathol 1985; 48: 207-217. 8. Wu SL, Fishman IJ, Shanon RL.: Chromophobe renal cell carcinoma with extensive calcification and ossification. Ann of Diag pathol 2002; 6(4): 244-247. 9. Prasad SR, Humphrey PA, Jay R et al.: Common and uncommon histologic subtype of renal cell carcinoma: imaging spectrum with pathologic correlation. Radiographics 2006; 26: 1795-1810. 10. Vera-Badillo FE, Conde E, Duran I.: Chromophobe renal cell carcinoma: a review of an uncommon entity. Int J Urol 2012; 19(10): 894-900. 11. Motzer RJ, Bacik J, Mariani T et al.: Treatment outcome and survival associated with metastatic renal cell carcinoma of non-clear-cell histology. J Clin Oncol 2002; 20: 2376-2381. 12. Larkin JM, Fisher RA, Pickering LM et al.: Chromophobe renal cell carcinoma with prolonged response to sequential sunitinib and everolimus. J Clin Oncol. 2011; 29: e241-242. 13. Klatte T, Han KR, Said JW et al.: Pathobiology and prognosis of chromophobe renal cell carcinoma. Urol Oncol 2008; 26: 604-609. 14. Choueiri TK, Plantade A, Elson P et al.: Efficacy of sunitinib and sorafenib in metastatic papillary and chromophobe renal cell carcinoma. J Clin Oncol 2008; 26: 127-131. 15. Zardavas D, Meisel A, Samaras P et al.: Temsirolimus is highly effective as third-line treatment in chromophobe renal cell cancer. Case Rep Oncol 2011; 4: 16-18.