Nieszczelność po rękawowej resekcji żołądka. Leczenie endoskopowe z zastosowaniem kleju tkankowego – opis przypadku
Leak after sleeve gastrectomy. Endoscopic treatment with the use of fibrin sealant – case report
Department of General, Oncological and Digestive Tract Surgery, Medical Centre of Postgraduate Education, Warszawa
Head of Department: prof. Wiesław Tarnowski, MD, PhD
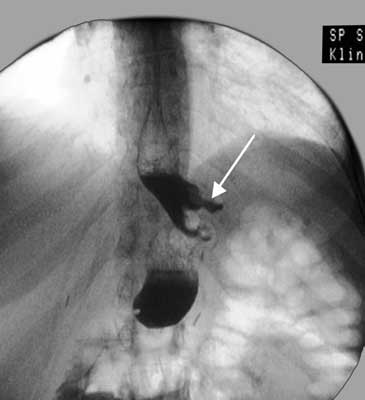
The prevalence of laparoscopic techniques favors the development of bariatric surgery. Minimally invasive techniques are associated with fewer complications and lower mortality in the perioperative period and laparoscopic access is currently preferred in bariatric surgery (1-3). Among the many methods of surgical treatment of obesity, sleeve gastrectomy is becoming increasingly popular. Over the last decade, sleeve gastrectomy has become one of the most frequently performed bariatric procedures and the effectiveness and safety of this method has been confirmed in numerous reports (4-8). The most feared complications associated with sleeve gastrectomy include leakage within the staple line. There are different theories on the causes of the leakage within the staple line after sleeve gastrectomy. A number of different methods of treatment were described in the case of this complication. In this paper, we will present a case of a patient in whom there was a leakage resulting from cutting the bougie used to calibrate the sleeve, and fibrin sealant, applied endoscopically, was used in the treatment.
1. Fried M, Hainer V, Basdevant A et al.: Inter-disciplinary European guidelines on surgery of severe obesity. Int J Obes 2007; 31: 569-577.
2. Reoch J, Mottillo S, Shimony A et al.: Safety of laparoscopic vs open bariatric surgery: a systematic review and meta-analysis. Arch Surg 2011; 146: 1314-1322.
3. Mechanick JI, Youdim A, Jones DB et al.: Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic Bariatric Surgery. Obesity 2013; suppl. 1: S1-27.
4. Buchwald H, Oien DM: Metabolic/Bariatric Surgery Worldwide 2011. Obes Surg 2013; 23: 427-436.
5. Gagner M, Deitel M, Kalberer TL et al.: The Second International Consensus Summit for Sleeve Gastrectomy, March 19-21, 2009. Surg Obes Relat Dis 2009; 5: 469-475.
6. Bellanger DE, Greenway FL: Laparoscopic sleeve gastrectomy, 529 cases without a leak: short-term results and technical considerations. Obes Surg 2011; 21: 146-150.
7. Bobowicz M, Lehmann A, Orlowski M et al.: Preliminary outcomes 1 year after laparoscopic sleeve gastrectomy based on Bariatric Analysis and Reporting Outcome System (BAROS). Obes Surg 2011; 21: 1843-1848.
8. Gagner M, Deitel M, Erickson AL et al.: Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy. Obes Surg 2013; 23: 2013-2017.
9. Chang SH, Stoll CR, Song J: The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis. 2003-2012. JAMA Surg 2014; 149: 275-287.
10. Buchwald H, Oien DM: Metabolic/bariatric surgery Worldwide 2008. Obes Surg 2009; 19: 1605-1611.
11. Hollenbeak CS, Rogers AM, Barrus B et al.: Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery 2008; 144: 736-743.
12. Zevin B, Aggarwal R, Grantcharov TP: Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 2012; 256: 60-71.
13. Markar SR, Penna M, Karthikesalingam A et al.: The impact of hospital and surgeon volume on clinical outcome following bariatric surgery. Obes Surg 2012; 22: 1126-1134.
14. Sanni A, Perez S, Medbery R et al.: Postoperative complications in bariatric surgery using age and BMI stratification: a study using ACS-NSQIP data. Surg Endosc 2014; 28: 3302-3309.
15. Hutter MM, Schirmer BD, Jones DB et al.: First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg 2011; 254: 410-420; discussion 420-422.
16. Zhang C, Yuan Y, Qiu C et al.: A meta-analysis of 2-year effect after surgery: laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for morbid obesity and diabetes mellitus. Obes Surg 2014; 24: 1528-1535.
17. Frezza EE, Reddy S, Gee LL et al.: Complications after sleeve gastrectomy for morbid obesity. Obes Surg 2009; 19: 684-687.
18. Brethauer SA, Hammel JP, Schauer PR: Systematic review of sleeve gastrectomy as staging and primary bariatric procedure. Surg Obes Relat Dis 2009; 5: 469-475.
19. Burgos AM, Braghetto I, Csendes A et al.: Gastric leak after laparoscopic-sleeve gastrectomy for obesity. Obes Surg 2009; 19: 1672-1677.
20. Fuks D, Verhaeghe P, Brehant O et al.: Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery 2009; 145: 106-113.
21. Aurora AR, Khaitan L, Saber AA: Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc 2012; 26: 1509-1515.
22. Lalor PF, Tucker ON, Szomstein S et al.: Complications after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 2008; 4: 33-38.
23. Dapri G, Cadière GB, Himpens J: Reinforcing the staple line during laparoscopic sleeve gastrectomy: prospective randomized clinical study comparing three different techniques. Obes Surg 2010; 20: 462-467.
24. Choi YY, Bae J, Hur KY et al.: Reinforcing the staple line during laparoscopic sleeve gastrectomy: does it have advantages? A meta-analysis. Obes Surg 2012; 22: 1206-1213.
25. Gagner M, Buchwald JN: Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis 2014; 10: 713-723.
26. Albanopoulos K, Alevizos L, Flessas J et al.: Reinforcing the staple line during laparoscopic sleeve gastrectomy: prospective randomized clinical study comparing two different techniques. Preliminary results. Obes Surg 2012; 22: 42-46.
27. Al Hajj GN, Haddad J: Preventing staple-line leak in sleeve gastrectomy: reinforcement with bovine pericardium vs. oversewing. Obes Surg 2013; 23: 1915-1921.
28. Yuval JB, Mintz Y, Cohen MJ et al.: The effects of bougie caliber on leaks and excess weight loss following laparoscopic sleeve gastrectomy. Is there an ideal bougie size? Obes Surg 2013; 23: 1685-1691.
29. Goitein D, Goitein O, Feigin A et al.: Sleeve gastrectomy: radiologic patterns after surgery. Surg Endosc 2009; 23: 1559-1563.
30. Casella G, Soricelli E, Rizello M et al.: Nonsurgical treatment of staple line leaks after laparoscopic sleeve gastrectomy. Obes Surg 2009; 19: 821-826.
31. Pequignot A, Fuks D, Verhaeghe P et al.: Is there a place for pigtail drains in the management of gastric leaks after laparoscopic sleeve gastrectomy? Obes Surg 2012; 22: 712-720.
32. Serra C, Baltasar A, Andreo L et al.: Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy. Obes Surg 2007; 17: 866-872.
33. Vix M, Diana M, Marx L et al.: Management of staple line leaks after sleeve gastrectomy in a consecutive series of 378 patients. Surg Laparosc Endosc Percutan Tech 2015; 25: 89-93.
34. Tan JT, Kariyawasam S, Wijeratne T et al.: Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg 2010; 20: 403-409.
35. Eubanks S, Edwards CA, Fearing NM et al.: Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg 2008; 206: 935-938; discussion 938-939.
36. Galloro G, Magno L, Musella M et al.: A novel dedicated endoscopic stent for staple-line leaks after laparoscopic sleeve gastrectomy: a case series. Surg Obes Relat Dis 2014; 10: 607-611.
37. Simon F, Siciliano I, Gillet A et al.: Gastric leak after laparoscopic sleeve gastrectomy: early covered self-expandable stent reduces healing time. Obes Surg 2013; 23: 687-692.
38. Alazmi W, Al-Sabah S, Ali DA et al.: Treating sleeve gastrectomy leak with endoscopic stenting: the kuwaiti experience and review of recent literature. Surg Endosc 2014; 28: 3425-3428.
39. Odemis B, Beyazit Y, Torun S et al.: Endoscopic closure of gastrocutaneous fistula with an AMPLATZER™ septal occluder device. Therap Adv Gastroenterol 2015; 8: 239-242.
40. Mercky P, Gonzalez JM, Aimore Bonin E et al.: Usefulness of over-the-scope clipping system for closing digestive fistulas. Dig Endosc 2015; 27: 18-24.
41. Papavramidis TS, Kotzampassi K, Kotidis E et al.: Endoscopic fibrin sealing of gastrocutaneous fistulas after sleeve gastrectomy and biliopancreatic diversion with duodenal switch. J Gastroenterol Hepatol 2008; 23: 1802-1805.
42. Baltasar A, Serra C, Bengochea M et al.: Use of Roux limb as remedial surgery for sleeve gastrectomy fistulas. Surg Obes Relat Dis 2008; 4: 759-763.
43. Szewczyk T, Janczak P, Janiak A et al.: Laparoscopic sleeve gastrectomy – 7 years of own experience. Wideochir Inne Tech Malo Inwazyjne 2014; 9: 427-435.
44. Ramos AC, Ramos MG, Campos JM et al.: Laparoscopic total gastrectomy as an alternative treatment to postsleeve chronic fistula. Surg Obes Relat Dis 2015; 11: 552-556.
45. Eisenberg D, Bellatorre A, Bellatorre N: Sleeve gastrectomy as a stand-alone bariatric operation for severe, morbid, and super obesity. JSLS 2013; 17: 63-67.