Monika Jabłońska-Jesionowska, *Lidia Zawadzka-Głos
Hypohidrotic ectodermal dysplasia as a rare cause of chronic rhinitis in children
Department of Pediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Summary
Introduction. Chronic rhinitis in children may have different causes, both local – with changes being present only in the nasal cavity – or systemic, with nasal congestion as one of the symptoms of a bigger clinical picture.
Aim. The aim of this study was to draw attention to a very rare congenital cause of chronic rhinitis in children – which is hypohidrotic ectodermal dysplasia.
Material and methods. A 6-month-old boy was admitted to the Department of Pediatric Otolaryngology of Warsaw Medical University due to chronic nasal obstruction present from birth. Clinical investigation included anterior and posterior rhinoscopy and fiberoscopy of nasopharynx. The MRI was also performed before admission. Complete blood count, serum iron level, serum thyroid hormones and level of IgG, IgA, IgM were examined to exclude anaemia, ozaena and hypothyroidism. Antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies (ANCA) tests were also ordered to exclude granulomatosis with polyangiitis. Next, a mucosal biopsy of the nasal cavity was performed to exclude primary ciliary dyskinesia. Allergic prick tests were also performed.
Results. After genetic tests, hypohidrotic ectodermal dysplasia was diagnosed.
Conclusions. 1. Every case of chronic nasal congestion in children requires not only adequate treatment, but also thorough clinical investigation. 2. Nasal obstruction may be due to local causes, systemic diseases and genetic disorders. 3. Hypohidrotic ectodermal dysplasia is a very rare genetic disorder that causes severe, even life threatening symptoms, one of which is chronic rhinitis.
INTRODUCTION
Chronic rhinitis in children may have different causes, both local – with changes being present only in the nasal cavity – or systemic, with nasal congestion as one of the symptoms of a bigger clinical picture (1, 4, 10). The causes of rhinitis differ with age. In infancy, congenital defects must be taken into account. Adequate nasal patency is important in the life of a child, especially in a newborn, as the inability to breathe through the nose is life threatening for a newborn. It can also cause problems in eating and developmental problems. The primary goal of a physician should be to achieve nasal patency in a child. Effective treatment depends on the correct diagnosis.
AIM
The aim of this study was to draw attention to a very rare congenital cause of children chronic rhinitis, which is hypohidrotic ectodermal dysplasia.
MATERIAL AND METHODS
A 6-month-old boy was admitted to the Department of Pediatric Otolaryngology of Warsaw Medical University due to chronic nasal obstruction present from birth. The child had been repeatedly hospitalized in pediatric and otolaryngology wards due to crusting in nasal cavities and drying of nasal discharge. As part of the clinical investigation, a swab from the nose was performed. Staphylococcus aureus MSSA, sensitive to cloxacillin, penicillin inhibitors, cephalosporins, and carbapenems, was cultured. The child had been treated locally by moisturizing, inhalations, nasal lavage with saline, topical Bactroban given periodically with temporary improvement. The nasal cavity was purified mechanically. The article presents diagnostic problems and treatment issues in this patient.
RESULTS
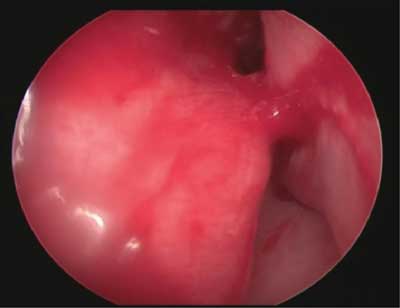
On the day of admission, the following findings in clinical examination were noted: dried discharge in the nasal cavities (fig. 1), complete nasal obstruction, deviation of nasal septum, bifurcated uvula and submucous cleft palate. Moreover, body mass deficiency, increased muscle tension and a slight delay in motor development were observed. The child was still not able to sit unsupported. The boy was under care of a neurologist. MRI of the brain showed no significant changes. In the hospital, differential diagnostic process of local and general causes of chronic rhinitis was performed. The tests for hypothyroidism, ozaena, granulomatosis with polyangiitis were performed. Thyroid hormones and iron levels were within normal limits and complete blood count was normal. Antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies (ANCA) were not detected. The results of urinalysis, serum creatinine, liver enzymes were within normal range. There were no pathological findings on chest X-ray. Brain MRI was assessed afresh in order to exclude craniofacial malformations in nose and nasopharynx. The deviation of nasal septum to the left and adenoid hypertrophy were found. Due to adenoid hypertrophy and submucous cleft palate, phoniatric consultation was ordered to assess the risk of palatopharyngeal insufficiency after an adenoidectomy which was considered. Choanal atresia and other malformations, such as meningocerebral hernia or hemangioma, were excluded. Nasal endoscopy in general anesthesia was performed to assess the anatomy of the region. Deviation of nasal septum to the left, adhesion of the septum and the middle nasal concha and a large adenoid were confirmed, and the adhesion was surgically removed (fig. 2). Due to the lack of phoniatric consent, adenoidectomy was not performed. To rule out primary ciliary dyskinesia, the biopsy of the nasal mucosa was taken and examined under electron microscope. The ciliar structure occurred to be correct.

Fig. 1. Massive crusts removed from the nasal cavity
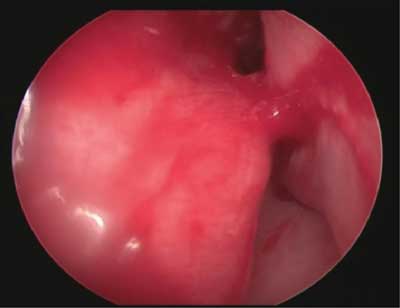
Fig. 2. Adhesion of septum and middle nasal concha in the nasal cavity
Local conservative treatment was continued with no improvement in nasal patency. Surgical treatment was considered. Due to the risk of palatopharyngeal insufficiency, there was no phoniatric consent for adenoidectomy. Septoplasty was contraindicated due to the age of the child. Palatoplasty was not indicated either.
The patient was readmitted to the Otolaryngology Department at the age of 9 months due to a significant nasal obstruction and episodes of decreased oxygen saturation, with minimal saturation being about 90%. The parents reported the necessity for mechanical suction of the nose two to three times a week in the otolaryngology outpatient department. Physical examination revealed crusty, drying nasal secretions and lack of teeth, as well as scarce hair on the head, very scarce eyebrows, dry skin, broad nasal bridge, and slightly slanted eyes. The boy’s weight was still too small for his age and he manifested a slight delay in motor development with the history of recurrent infections of the upper respiratory tract. He was referred to the genetics clinic. Due to the significant reluctance of the parents, who opined that nasal crusting was the child’s only problem, diagnostic process was completed eight months later. After the tests, the diagnosis of hypohidrotic ectodermal dysplasia was made.
DISCUSSION
Rhinitis is an inflammation of the nasal mucosa, characterized by at least one of the following symptoms: obstruction of the nose, nasal discharge, sneezing or itching (9). Symptoms must persist for at least for 1 hour a day on a significant amount of days in a year. Rhinitis actually comprises all the diseases of the nose that cause the impairment of its function. Causes of rhinitis can be divided into allergic, infectious, non-infectious, and other causes (9). The symptoms of allergic rhinitis manifest seasonally or year-round. Infectious rhinitis can be either acute or chronic, and it can have bacterial, viral or fungal etiology. Other causes of rhinitis include: NARES – nonallergic rhinitis with eosinophilia, drug-induced rhinitis, hormonal rhinitis, rhinitis caused by irritants, and mechanical rhinitis (10). In medical history gathered from pediatric patients and their parents, few factors are of highest importance: time of onset (since birth or acquired later), symptoms being intermittent or permanent and unilateral or bilateral. The causes of rhinitis are different depending on the age of the child (1, 4, 10). Causes of rhinitis in infants are shown in table 1 (2-5).
Tab. 1. Causes of rhinitis in infants
GERD (physiology, body position, overfeeding, artificial feeding, lactose intolerance)
Mechanical irritation; daily toilet with suction or sea salt products
Allergies
Infectious rhinitis; very rare to the 5th month of life (nursery, older siblings)
Congenital craniofacial defects:
– cleft palate, choanal atresia
– congenital syndromes: CHARGE, hypohidrotic ectodermal dysplasia
– narrowing the anterior nostrils
– congenital cyst of nasolacrimal duct
Congenital tumors of the nose:
– meningocerebral hernia
– glioma
– dermoidal cyst
Tumors of the nose:
– benign tumors: hemangioma
– malignant tumors – most often: rhabdomyosarcoma; rarely – lymphoma, neuroblastoma
Hormonal rhinitis:
– congenital hypothyroidism
– hypothyroidism in pregnancy of the mother
Mechanical rhinitis:
– anatomical changes (deviation of the nasal septum, malformations of the lateral wall of the nasal cavity)
– foreign bodies
– injuries
– adenoid hypertrophy
Other:
– drugs used by the mother during pregnancy and breastfeeding (narcotic drugs, antihypertensive drugs, antidepressants)
– rhinitis medicamentosa due to decongestant nasal drops |
Clinical investigation of a patient with chronic rhinitis includes anterior and posterior rhinoscopy with the assessment of nasal patency, e.g. with the help of a Politzer balloon. After that, nasal endoscopy and fiberoscopy of nasopharynx should be performed. In case of a tumor-like lesion, MRI or craniofacial CT with contrast is recommended. Next, a biopsy of pathological changes in the nasal cavity or mucosal biopsy is performed to exclude the primary ciliary dyskinesia. Additionally, complete blood count, serum iron level, serum thyroid hormones levels and serum levels of IgG, IgA, IgM are examined. If granulomatosis with polyangiitis is suspected, test on antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies (ANCA) is done. In some cases, allergy tests are also performed (4, 5). Only the correct diagnosis enables appropriate treatment. In this case, the reason for massive crusting in the nasal cavity was not found during the routine diagnostic process. The following hospitalization of the boy in his 9 months of age showed changes outside nasal cavity, which led us to recommend genetic testing in the patient. The features included: lack of hair, dark skin around the eyes, absence of the teeth, deficiency of body mass, motor retardation. Finally, the boy was diagnosed with hypohidrotic ectodermal dysplasia.
Hypohidrotic ectodermal dysplasia is an hereditary condition of the ectodermal tissue caused by a mutation in the EDA, EDAR, or EDARADD genes. It is usually an X-linked recessive disease (6-8). The condition is difficult to diagnose in infancy, because symptoms are unspecific and can affect the upper respiratory tract and digestive tract, as well as ectodermal tissues. The most characteristic symptoms include hypotrichosis (abnormal hair pattern; hair is thin and lightly pigmented), hypohidrosis (diminished sweating, in this case due to the reduction or absence of salivary glands), hypodontia (abnormal development of teeth), absence of lacrimal glands, and abnormal skin development. Hypohidrosis, which is present in most patients with hypohidrotic ectodermal dysplasia, can lead to hyperthermia, which can be life-threatening, especially in small, undiagnosed children. Physical growth and psychomotor development are normal (6-8). Laryngological features of this syndrome include: chronic respiratory tract infections, persistent nasal discharge with crusting, and hearing problems. Some children also have chronic eczema and periorbital hyperpigmentation. Other facial signs include depressed nasal bridge, thick lips, lack of dermal ridges, and a retruded chin. The diagnosis is often delayed, as it was the case with our patient, until problems with teeth development are noticed (6-8). Currently, no causal treatment for the disease is available. Protection from overheating and adequate water intake, as well as optimal room temperature, are of primary importance due to the risk of overheating. Dental prostheses should be provided and nasal and aural crusting should be regularly removed. Adequate air humidification can help in preventing crusting. Genetic tests performed in families with history of HED should be offered to enable early diagnosis and treatment, especially due to the risk of hyperthermia (6-8).
CONCLUSIONS
1. Every case of chronic nasal congestion in children requires not only adequate treatment, but also thorough clinical investigation.
2. Nasal obstruction may be due to local causes, systemic diseases and genetic disorders.
3. Hypohidrotic ectodermal dysplasia is a very rare genetic disorder that causes severe, even life threatening symptoms, one of which is chronic rhinitis.
Piśmiennictwo
1. Wei JL: Chronic nasal dysfunction in children: Allergic rhinitis? Infectious? What to do if neither? Curr Opin Otolaryngol Head Neck Surg 2015; 23(6): 491-498. 2. Choi S-H, Han M-Y, Young-Min Ahn Y-M et al.: Predisposing factors associated with chronic and reccurent rhinosinusitis in childhood. Allergy Asthma Immunol Res 2012; 4(2): 80-84. 3. Prokopakis E, Kalogjera L, Karatzanis A: Pediatric severe chronic upper airway disease (P-SCUAD). Curr Allergy Asthma Rep 2015; 15(12): 1-5. 4. Rose AS, Thorp BD, Zanation AM, Ebert CS: Chronic rhinosinusitis in children. Pediatr Clin North Am 2013; 60(4): 979-991. 5. Silviu-Dan F: Pediatric chronic rhinosinusitis. Pediatr Ann 2014; 43(8): e201-209. 6. Daniel E, McCurdy EA, Shashi V, McGuirt WF Jr: Ectodermal dysplasia: otolaryngologic manifestations and management. Laryngoscope 2002 Jun; 112(6): 962-967. 7. Wright T, Grange DK, Richter MK: Hypohidrotic ectodermal dysplasia synonyms. Anhidrotic Ectodermal Dysplasia, Christ-Siemens-Touraine Syndrome. J Initial Posting 2003; 28. Last Update: May 15, 2014. 8. Al-Jassim AH, Swift AC: Persistent nasal crusting due to hypohidrotic ectodermal dysplasia. J Laryngol Otol 1996 Apr; 110(4): 379-382. 9. Lund V: International Consensus Report on the diagnosis and management of rhinitis. International Rhinitis Management Working Group. Allergy 1994; 49: 1-34. 10. Hardjojo A, Shek LP, van Bever HP, Lee BW: Rhinitis in children less than 6 years of age: current knowledge and challenges. Asia Pac Allergy 2011 Oct; 1(3): 115-122.