Krzysztof Ślączka1, Marcin Dziekiewicz2, Monika Jabłońska-Jesionowska1, *Lidia Zawadzka-Głos1
Gastroesophageal reflux disease in children with recurrent croup
1Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
2Department of Pediatric Gastroenterology and Nutrition, Medical University of Warsaw, Poland
Head of Department: Piotr Albrecht, MD, PhD
Summary
Introduction. Episodic croup occurs most often in children between 0.5 and 3 years of age. Recurrent croup presents most often in older children. It shows an association with gastroesophageal reflux disease, allergy and laryngeal abnormalities.
Aim. The aim of this study was to explore the relationship between recurrent croup and gastroesophageal reflux disease in children with the history of at least one episode of severe croup.
Material and methods. The study included 22 children with recurrent croup admitted to the Department of Pediatric Otolaryngology of the Medical University of Warsaw between the years 2013 and 2016. Information concerning leading symptoms and medical history was obtained from the medical documentation of the patients. All the patients underwent rigid laryngoscopy and were diagnosed using 24-hours, single probe esophageal pH monitoring.
Results. 22 children aged between 1.5 year to 7.5 years were examined and their medical records were analyzed. An acid reflux was diagnosed in fourteen patients (63.6%) and the mean Reflux Index was 11.6. On endoscopic examination of the larynx, 15 patients (61.8%) had normal findings, 7 patients (31.8%) were diagnosed with an airway abnormality including: 3 cases of laryngeal cleft (type I), 2 cases of laryngomalacia, 1 case of subglottic stenosis, 1 case of vocal fold nodules. In 5 cases (22.7%), GERD coexisted with larynx abnormalities.
Conclusions. All the children with recurrent croup should be diagnosed for both gastroesophageal reflux disease and laryngeal abnormalities. Therefore, ENT specialists, as well as gastroenterologists, should take part in diagnostic procedures to reveal primary conditions responsible for recurrent croup.
INTRODUCTION
Croup is a common respiratory tract disease in children. It presents with an acute onset, hoarseness, inspiratory stridor, barking cough and respiratory distress (1). These symptoms are caused by the inflammation and narrowing of the subglottic area of the larynx, which is the narrowest part of the respiratory tract in children (2, 3). Infectious croup is typically caused by viruses, especially during fall and winter (4). It primarily affects children between 6 months and 3 years of age, with the peak incidence at two years of age (5). It is unusual for healthy children to have more than one episode of croup per year (6). However, when the croup-like episodes occur more than two times in a year, it is referred to as recurrent croup and its presence should alert clinician to investigate underlying reasons for it (tab. 1) (7).
Tab. 1. Risk factors for recurrent croup in children (11)
| Congenital | Congenital subglottic stenosis
Congenital cardiovascular abnormality
Tracheo-oesophageal fistula
Laryngotracheal cleft
Tracheobronchomalacia
Vocal cord paralysis
Congenital tracheal stenosis
Congenital goitre |
| Traumatic | Acquired subglottic stenosis
Subglottic cyst
Airway foreign body |
| Inflammatory | Gastroesophageal reflux disease
Asthma
Allergy |
| Infectious | Viral
Bacterial |
| Tumor | Subglottic haemangioma
Lymphangioma
Thyroid neoplasm
Recurrent respiratory papillomatosis
Thymoma
Lymphoma
Mediastinal mass |
Frequent croup episodes can be caused by a disease that narrows respiratory tract (6). Several recent studies have shown an association between recurrent croup and gastroesophageal reflux disease (GERD), laryngeal abnormalities, allergy, atopy, airway hyperreactivity and asthma (tab. 2) (8-10).
Tab. 2. Diseases and symptoms related to GERD in children (16)
| Upper respiratory tract | Lower respiratory tract | Digestive tract |
– subglottic
– stenosis
– laryngomalacia
– vocal cord
– nodules
– recurrent croup
– recurrent otitis media
– chronic rhinitis | – asthma
– recurrent
– papillomatosis
– wheezing | – eosinophilic esophagitis
– swallowing
– dysfunction
– vomiting
– burping |
Moreover, antireflux therapy in GERD-positive cases can successfully reduce the number and duration of croup-like episodes (11).
AIM
The aim of this study was to explore the relationship between recurrent croup and gastroesophageal reflux disease in children with the history of at least one episode of severe croup.
MATERIAL AND METHODS
The study was conducted on a group of pediatric patients with recurrent croup admitted to the Department of Pediatric Otolaryngology of Medical University of Warsaw between January 2013 and February 2016. Recurrent croup was defined as more than 2 episodes of croup-like syndrome per year. All children were admitted to the hospital due to an episode of severe croup (more than 6 points in Westley Croup Score) at least once in their lifetime. In most cases, the leading symptoms of croup episodes included inspiratory stridor, barking cough and inspiratory dyspnea. In the Department, each patient was treated using the same scheme, including i.v. steroids combined with nebulized steroids and adrenaline. The collected medical data included age, sex, symptoms, medical history, the number of croup episodes and hospitalizations for croup, as well as the number of emergency visits. All patients undergone rigid endoscopic laryngoscopy to inspect the airways from epiglottis to trachea. Reflux finding score (RFS) was then given based on the endoscopic examination. All the patients were investigated for GERD using 24-hour, single probe esophageal pH monitoring, which was placed at the level of the 2nd vertebra above the diaphragm (based on the X-ray scan). Based on the results of the examination, Reflux Index (RI) was calculated and acid gastroesophageal reflux disease was diagnosed or excluded. Children with diagnosed GERD were enlisted for the outpatient reflux treatment. They all subsequently achieved symptom-free status.
RESULTS
22 children between 1.5 year to 7.5 years of age were examined and their medical records were analyzed. The mean age at their first stay in our Department was 4.25 ± 1.85 years, with the youngest child being 22 months old and the oldest being 89 months old, and the mean age at the first croup episode was 7.8 ± 5.9 months. The male-to-female ratio was 2.1:1. The mean BMI was 16 ± 2 kg/m2. All the patients had had a history of at least one emergency room visit, as well as one hospital admission due to a croup episode. Sixteen children (72.7%) had had croup episodes more than three times a year and eight children (36.3%) had been hospitalized for croup more than once in their lifetime. Two children (9%) had a history of ICU hospitalization and one of them had been intubated in infancy (4.5%). Four children (18.1%) had had low birth weight and five children (22.7%) had been born prematurely before the completion of 37 weeks of gestational age. Seven patients (31.8%) had had at least one comorbidity: 2 children were diagnosed with atopic dermatitis, 4 – with allergy and asthma and 1 – with epilepsy.
An acid GER disease was found in fourteen patients (63,6%) and the mean RI in this group of children was of 11,6%, with RI > 4.5% being considered as positive. The mean BMI of patients diagnosed with GERD was 16 for both sexes and BMI was higher than 17 in only two children. Parents or legal guardians of children diagnosed with GERD were asked about their children’s dietary habits. 85% of children “very often” consumed a type of food that is considered unhealthy (full-fat cheese, white bread, sweets, fast-food and snacks). Only in 3 cases, the parents admitted to carefully avoiding saturated fats and high-calorie snacks and replacing it with a healthy diet: vegetables, fruit and dairy.
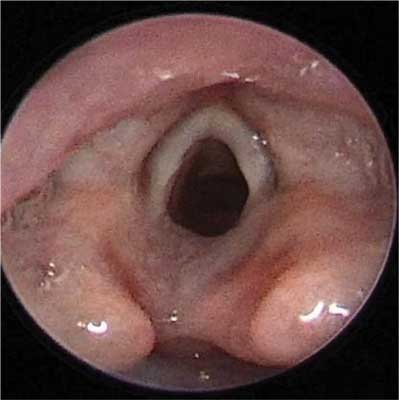
On endoscopic examination of the larynx, 15 patients (61.8%) had normal findings, 7 patients (31.8%) were diagnosed with an airway abnormality including: 3 cases of laryngeal cleft (type I) (fig. 1), 2 cases of laryngomalacia (fig. 2), 1 case of subglottic stenosis (fig. 3), 1 case of vocal fold nodules (fig. 4). In 5 cases (22.7%), GERD coexisted with larynx abnormalities.
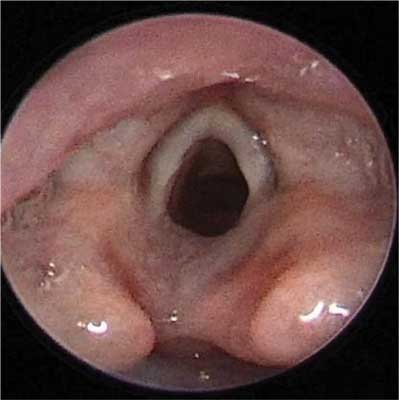
Fig. 1. Laryngeal cleft

Fig. 2. Laryngomalacia

Fig. 3. Subglottic stenosis

Fig. 4. Vocal fold nodules
However, mean RFS of GERD patients was 4.8 ± 2.4, which suggests that GERD-related symptoms do not always lead to mucosal lesions in larynx. In our study, 50% of the patients had endoscopic findings corresponding to ≥ 7 in RFS (tab. 3).
Tab. 3. GERD and laryngeal abnormalities
| Pediatric patients with recurrent croup (n = 22) |
| GERD: 14 (of 22; 63.6%) | laryngeal abnormalities 7 (of 22; 31.8%) |
mean RI%: 11.6%
F: 6 (of 7; 85%)
M: 8 (of 15; 50%)
age < 4 years: 14 (of 22; 63.6%)
age > 4 years: 8 (of 22; 36.4%)
mean BMI: 16 | laryngeal cleft 3 (of 22)
laryngomalacia 2 (of 22)
subglottic stenosis 1 (of 22)
vocal fold nodules 1 (of 22)
mean RFS: 4.6 points
RFS ≥ 7 in 50% of the cases |
DISCUSSION
Croup is a common and benign childhood disease, but it is unlikely to present more than once or twice a year. Virus infection and edematous inflammation of the subglottic area are responsible for the majority of episodic cases. However, in recurrent spasmodic disease, contributing and/or underlying conditions should be investigated. Our results mostly correspond with the results of other studies (2, 8, 9, 11). Our inclusion criterion was at least one hospital admission due to croup episode, as, in our opinion, it helps to enroll patients who had undergone a severe course of the illness. However, other researchers did not proceed in this way (9).
In our study, male-to-female ratio was 2.1:1. Other researchers have also noted higher prevalence of croup in male patients (11, 2). We also observed that 22.7% of our patients had been born preterm, which corresponds to 20% of preterm children noted in a study by Cooper et al. (2). In the study mentioned, 11.5% of patients had had been intubated because of croup, whereas in our group, only one patient had been intubated (4.5%). In our study, the age at the first croup episode ranged from 1.5 months to 2 years. Similar data was gathered in other studies (2, 8, 10). Mean age at the first visit in our Department was 4.25 ± 1.85 years, which complies to the results of studies by Kwong et al. and Arslan et al. A recurrent croup can develop at any age, even in children younger than 6 months or older than 3 years (6). It may be hypothesized that the recurrence of croup in older age is due to secondary reasons triggering croup episodes (8, 10). In our study, 63.6% of the patients had both recurrent croup and gastroesophageal reflux disease. 31.8% of our patients had laryngeal abnormalities and 22.7% of the patients were diagnosed with both GERD and laryngeal abnormalities. We found that not every patient with acid reflux had GERD-related lesions on laryngeal mucosa. In our study, only half of patients had this type of endoscopic findings in larynx. In a study from 2007, Kwong et al. stated that 82.3% of the patients with recurrent croup had had laryngoscopic and bronchoscopic findings of acid GERD and laryngopharyngeal reflux (LPR) (10). However, the researchers suggest GERD patients may have been underdiagnosed in the study, because only 35% of their patients were diagnosed with acid reflux. The opposite was true for our research, where only 50% of patients had GERD-related lesions on endoscopy. In our study, the children underwent a single probe esophageal pH monitoring. In 1992, Contencin and Narcy conducted a small study on 8 children, in which combined pharyngeal and esophageal pH monitoring was used. All the patients with recurrent croup were diagnosed with acid GERD (12). We found that children with acid reflux have a higher prevalence of laryngeal lesions than the healthy population. A systematic review revealed that there is a relationship between acid reflux and laryngomalacia, but the association is not causal (13). Similarly, Rankin et al. describe a group of 90 children, 28% of which had anatomical airway abnormalities, and 26% had GERD-related laryngeal lesions in microlaryngoscopy (14). Likewise, Greifer et al. reviewed 40 cases of recurrent croup, 53% of which had airway anomalies and 38% had esophagitis in biopsy (15).
In 1995, Waki et al. discovered that children with 2 episodes of croup a year are less likely to develop acid reflux disease than children with 3 or more episodes, with the percentage of children developing GERD being 47 and 63%, respectively (9). In our group, having had more than 2 episodes of croup a year was one of the inclusion criterion. Therefore, there was no children with 2 episodes of croup in our study. However, using similar methodology, we have discovered only three cases (21.4%) of children diagnosed with acid reflux having no more than 3 episodes a year. Similarly, there were eleven cases (78.6%) of children with GERD that had had 4 or more episodes a year. We may conclude that in our study, children having 4 or more episodes a year were more likely to develop acid reflux.
We found that six out of seven female participants in our study had reflux disease, and two thirds of them were 2 to 3 years old. Eight out of fifteen boys were diagnosed with GERD, and six of them were 2 to 3 years old. Our study included twice as many boys suffering from recurring croup as girls, however, girls were diagnosed with GERD nearly two times more often. These findings could not be compared to any available medical literature. Further research is needed to confirm this finding.
BMI was normal for most of the children participating in our study. Only 18.3% of children, both male and female, were above the 50th percentile in BMI-for-age charts. Moreover, only half of those patients had typical history of chronic symptoms, such as regurgitation, cough, vomiting, heartburn or abdominal pain. In our group, 85% of children regularly consumed unhealthy food. This subgroup showed high prevalence of GERD, which may be related to the consumption of unhealthy food, but further studies are needed on this subject. We did not find medical literature describing dietary habits of children diagnosed with both recurrent croup and acid reflux. What is more, we have not yet found any research concerning prevalence of recurrent croup and GERD in Polish children.
CONCLUSIONS
1. Pediatric patients with recurrent croup should be diagnosed for gastroesophageal reflux disease.
2. Airway anomalies are common in children with recurrent croup.
3. Recurrent croup in children is rarely a subject of research in Poland.
4. ENT specialists and gastroenterologists should have an active role in determining primary reasons for recurrent croup.
Piśmiennictwo
1. Bjornson CL, Johnson DW: Croup. Lancet 2008; 371: 329-339. 2. Cooper T, Kuruvilla G, Persad R et al.: Atypical croup:association with airway lesions, atopy, and esophagitis. Otolaryngol Head Neck Surg 2012 Aug;147(2): 209-214. 3. Harless J, Ramaiah R, Bhananker SM: Pediatric airway management. Int J Crit Illn Inj Sci 2014 Jan-Mar; 4(1): 65–70. 4. Knutson D, Aring A: Viral croup. Am Fam Physician 2004 Feb 1; 69(3):535-540. 5. Rittichier KK, Ledwith CA: Outpatient treatment of moderate croup with dexamethasone: intramuscular versus oral dosing. Pediatrics 2000 Dec; 106(6):1344-1348. 6. Joshi V, Malik V, Mirza O et al.:Fifteen-minute consultation: structured approach to management of a child with recurrent croup. Arch Dis Child Educ Pract Ed 2014 Jun; 99(3): 90-93. 7. Farmer TL, Wohl DL: Diagnosis of recurrent intermittent airway obstruction ("recurrent croup") in children. Ann Otol Rhinol Laryngol 2001 Jul; 110(7 Pt 1): 600-605. 8. Arslan Z, Cipe FE, Ozmen S et al.: Evaluation of allergic sensitization and gastroesophageal reflux disease in children with recurrent croup. Pediatr Int 2009 Oct; 51(5): 661-665. 9. Waki EY, Madgy DN, Belenky WM et al.: The incidence of gastroesophageal reflux in recurrent croup. Int J Pediatr Otorhinolaryngol. 1995 Jul; 32(3):223-232. 10. Kwong K, Hoa M, Coticchia JM: Recurrent croup presentation, diagnosis, and management. Am J Otolaryngol 2007 Nov-Dec; 28(6): 401-407. 11. Hoa M, Kingsley EL, Coticchia JM: Correlating the clinical course of recurrent croup with endoscopic findings: a retrospective observational study. Ann Otol Rhinol Laryngol. 2008 Jun; 117(6): 464-469. 12. Contencin P, Narcy P: Gastropharyngeal reflux in infants and children. A pharyngeal pH monitoring study. Arch Otolaryngol Head Neck Surg 1992 Oct; 118(10): 1028-1030. 13. Hartl TT, Chadha NK: A systematic review of laryngomalacia and acid reflux. Otolaryngol Head Neck Surg 2012 Oct; 147(4): 619-626. Epub 2012 Jun 27. 14. Rankin I, Wang SM, Waters A et al.: The management of recurrent croup in children. J Laryngol Otol 2013 May;127(5): 494-500. 15. Greifer M, Santiago MT, Tsirilakis K et al.: Pediatric patients with chronic cough and recurrent croup: the case for a multidisciplinary approach. Int J Pediatr Otorhinolaryngol 2015 May; 79(5): 749-752. 16. Venkatesan NN, Pine HS, Underbrink M.: Laryngopharyngeal reflux disease in children. Pediatr Clin North Am 2013 Aug; 60(4): 865-78. doi: 10.1016/j.pcl.2013.04.011.