© Borgis - New Medicine 2/2002, s. 76-79
Ivo Marik1, K Kozlowski2
Frontometaphyseal dysplasia in a 3 5/12 year-old girl and in the „unaffected mother”
1Ambulant Centre for Defects of Locomotor Apparatus, Prague, Czech Republic
2Royal Alexandra Hospital for Children, Sydney, Australia
Summary
We report a girl with fromtometaphyseal dysplasia in whom the first phenotypic abnormality noted at the age of 3 months was metopic suture torus. At the end of the first year of life knock knee deformity and torsion of the legs was noted and this progressed in spite of orthotic treatment. The diagnosis of frontometaphyseal dysplasia was established at the age of 3 years 5 months. Family studies revealed that the mother, supposed to be normal was also affected. Previously unreported clinical manifestations and radiographic findings are documented to further delineate and expand the spectrum of the disorder.
INTRODUCTION
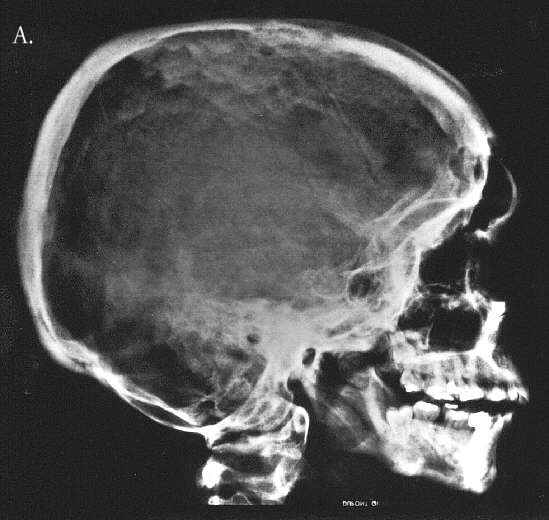
Frontometaphyseal dysplasia (FMD) is an uncommon disorder diagnosed rarely at preschool age. We report a girl in whom the first abnormality was a metopic suture torus recognised at the age of 3 months. Knock knee deformity and twisted legs were noted at the end of the first year of life. The mother showed mild expressivity of the disease and was regarded as normal until the diagnosis was made in her daughter (Fig 1A).

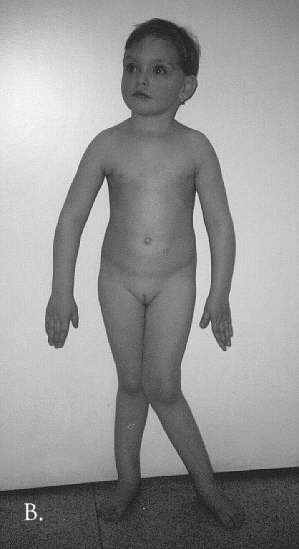
Fig. 1A & B. A. Facial appearance of the proband at the age of 4 1/2 years and the mother at the age of 25 years. Note prominent supraorbital ridges in both the mother and the daughter and the metopic torus in the proband. B. Proband at the age of 3 1/2 years. Severe left sided coxa valga. Minor right sided coxa valga with lateral bowing of the right leg.
CASES REPORT
This Czech girl was born at 36 weeks of gestation to a 24 year old, gravida 1 para 1 mother and a healthy father. The pregnancy was complicated by phlebothrombosis of the left lower extremity with low molecular heparin. Birth weight and length were 2800 g and 49 cm respectively. She required oxygen, drip feeding and antibiotics for the first five days of live because of anaemia and possible sepsis related to the pregnancy. Ultrasound examination disclosed a Grade I subependymal haemorrhage and an atrial septal defect which closed spontaneously. At the age of 3 months a hard, bony prominence along the metopic suture, and in the last few months of the first year of life, progressive knock knee and leg deformities were noted. The latter gradually increased under observation in the next few years of life in spite of orthotic treatment. Her psychomotor development in the first few years of life was normal. At the age of 3 years some kind of metaphyseal dysplasia was diagnosed at the Genetic Department in Ostrava.
She was examined at the Centre for Patients with Defects of the Locomotor System in Prague at the age of 3 years and 5 months (Fig 1B). Her height was 103 cm (75 centile), weight 17 kg (90 centile), head circumference 50 cm (75 centile), chest circunference 57 cm (65 centile). There was bilateral knock knee deformity with torsion of the legs more marked on the left. The range of hip motion and knee flexion was decreased. Her extremities were relatively long in comparison with the trunk. There was scoliosis secondary to leg asymmetry. She had an unusual facial appearance; this was characterised by a high forehead with a prominence along the metopic suture and prominence of the supra-orbital ridges. There was mild hypertelorism, exophthalmos and bilateral epicanthus. The philtrum was long and the chin was small. There was diastasis between the incisors and the teeth were hypoplastic. She had brown straight hair. Her mental development was normal. Inspite of orthotic treatment her leg deformities progressed. At the age of 6 years her height was 119.7 cm (50-75 centile, weight 26 kg (90 centile). Examination of proportions disclosed long upper (+1.5 SD) and lower (+2 SD) extremities. The neck was short (-1.2 SD) and the shoulders relatively narrow (-0.6 SD). The pelvis (+2.5 SD) and the thorax (+1.5 SD) were broad. The skull was scaphocephalic. Head circumference was 52.3 cm (75-90 centile). Her mental development was normal. Her hearing was not affected.
Extensive biochemical investigations specifically those of Ca/P metabolism were normal.
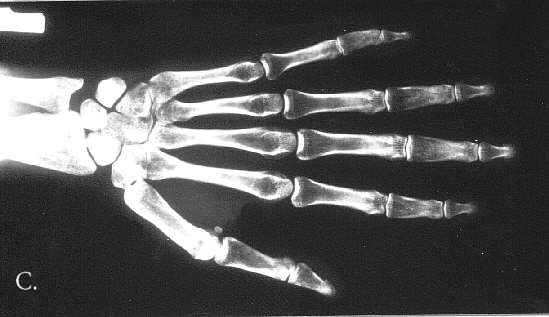
Radiographic examination documented changes characteristic of frontometaphyseal dysplasia. In the skull the density of the base of the skull and od the mid-frontal bone area was increased. The frontal sinus was absent. The teeth were hypoplastic/dysplastic. The ribs were thin and slightly irregular in contour. The scapulae were large, slightly dysplastic with prominent acromion processes. The bodies of the iliac bones were small and there was flaring of the iliac wings. There was bilateral coxa valga. There was a mild undertubulation of the metaphyses of all the long bones which were also slightly bowed. The tibiae were most severly affected and showed S-like deformity in the lateral projection. The patellae were small. The spine was normal and the hands were little affected (Fig 2 A-D).




Fig. 2A-D. Thin cortex, abnormal, indistinctive trabecular pattern. A. 5 10/12 year old. Thin ribs. Wavy deformity of the 12-th rib. B. 6 year-old. Flaring of iliac bones, coxa valga. C. 4 10/12 year-old. S-like deformity of the tibia, more marked on the right. Small patellae. D. 6 year-pld. Hypotubulation of the phalanges. Middle phalanges are most severly affected. Minimal dysplastic changes in the carpals and metacarpals. Bone age equals chronological age.
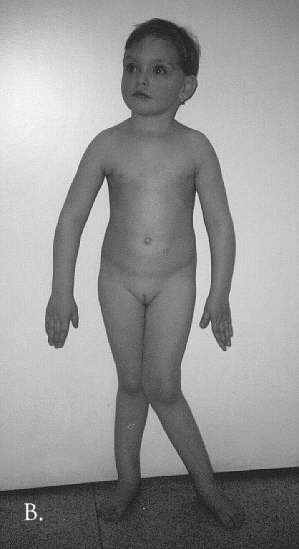
Case II – The mother of case I had a facial appearance similar to her daughter. Her height was 162 cm, weight 56 kg. She had a slight knock knee deformity but no twisting of the legs and her gait was almost normal. Radiographs of the pelvis, skull and left hand documented changes consistent with FMD (Fig 3A-C).
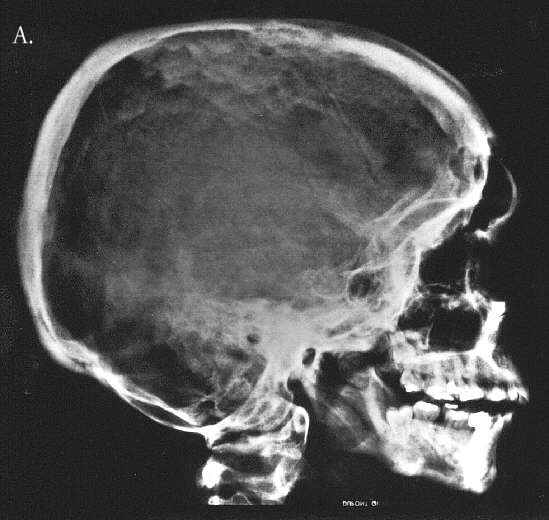

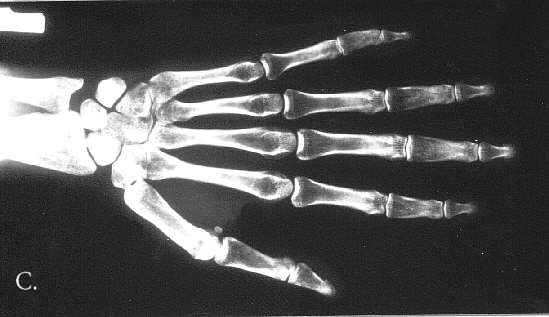
Fig. 3A-C. 25 year-old. A. Hyperostosis of the cranial vault and base and of facial bones, perisutural sclerosis, abnormal alignement in atlanto-occipital region, minute frontal sinus, poorly pneumatised mastoids, prominent supraorbital ridges, hypoplastic maxilla and mandible, micodontia. B. Flared ilia, small iliac bodies, expanded ischial bones, coxa valga with broad femoral necks. C. Hypotubulation of the middle phalanges.
DISCUSSION
FMD was delineated as a separate entity by Gorlin and Cohen in 1969 (1). The salient features were marked supraorbital ridges, agenesis of frontal sinuses, underdeveloped mandible, hearing loss, joint contractures, splayed metaphyses of the long bones, and flaring iliac bones. Up to 1994 about 35 cases had been reported (2), however some patients were reported more than once (3-11). Inheritance of the disorder has been claimed to be both X-linked and autosomal dominant (5, 8).
The diagnosis of FMD is easy for the observer who knows the disorder. The unique facial features and characteristic radiographic appearances do not allow confusion with other craniotubular disorders (12-14). However the signs and symptoms of FMD which are latent or amorphous in the early period of life as in all craniotubular dysplasias manifest increasingly distinctive features with advancing age (15). A patient regarded as normal at birth can be severely affected in the teens or early adulthood. Even if abnormal facial appearances, hand and foot deformities are noted at birth their proper syndromic association is not recognised. The difficulties in diagnosis later in life are the result of its rarity, unfamiliarity with the characteristic facial features and very variable clinical presentation. Patients whose expressivity of the disease is on a small scale may by regarded as normal. Therefore, as we have been stressing for years, a skeletal survey sent for consultation should be accompanied by a photograph of the patient. The mother of our case I whose physical appearance was hardly modified was thought to be normal until FMD was diagnosed in her daughter. Case I was regarded as normal at birth. To the best of our knowledge metopic suture torus as the first clinical abnormality was not yet reported in FMD. We postulate that it was present for at least some weeks or even months before being noted at the age of 3 month. Although genu valgum of minor degree is a common finding in FMD, early progressive genu valgum resistant to orthotic treatment is an unusual complication. At the age of 3 years and 5 months she presented diagnostic facial appearances and characteristic radiographic findings. It is worth stressing that our patient did nor have hand and feet deformities a common accompaniment of FMD.
Case II had same facial appearance as her daughter (Fig 1). The radiographs of the skull, pelvis and hand confirmed the diagnosis of FMD (Fig 3A-C).
The clinico-radiographic appearances of FMD are so characteristic that, if all the clinical data and full skeletal survey are available, no confusion can occur, except in the differential diagnosis with other cranio-tubular dysplasias in the first few years of life (15). All of them have different facial appearances and different radiographic features.
Craniometaphyseal dysplasia (13, 14) is characterised by paranasal bossing, prognathism and recurrent transient facial palsy. Sclerosis of skull is more uniform and more advanced. Widening of the metaphyses is more salient than in FMD. Pelvis and ribs show borderline to minimal dysplastic changes.
Progressive distortion of the face (leontiasis ossea) with marked paranasal bossing, flattening of he nasal bridge, compression of the cranial nerves, with obstruction of the nasal airways and lacrimal ducts typify Craniodiphyseal dysplasia (13, 14). Major radiographic signs consist of hyperostosis of the skull, diaphyseal expanson with sclerosis and widening of the ribs and clavicles.
Both craniometaphyseal and craniodiaphyseal dysplasia have different cranial appearances from FMD, with major deformity in the mid-facial region Other cranio-tubular dysplasias (13, 14) such as osteodysplasty (Melnick-Needles syndrome), dysosteosclerosis, sclerosteosis, endosteal hyperostosis (van Buchem and Worth types) and osteopathia striata present such different clinical appearances and radiographic findings that one is unlikely to confuse them with CMD.
CONCLUSION
New features of FMD are reported in early life, metopic torus in the neonatal period and early severe, progressive genu valgum after one year. Family studies of a dysmorphic child may help to establish a diagnosis before characterictic signs and symptoms develop.
Piśmiennictwo
1. Gorlin R.J., Cohen M.M.: Frontometaphyseal dysplasia. A new syndrome. Am. J. Dis. Child. 1969, 118:487-494. 2. Taybi H., Lachmann R.S.: Radiology of syndromes, metabolic disorders and skeletal dysplasias. 4th edn. Year Book, Chicago 1996, 821-823. 3. Holt J.F. et al.: Frontometaphyseal dysplasia. Radiol. Clin. North Am. 1972, 10:225-243. 4. Danks D.M. et al.: Fronto-metaphyseal dysplasia. Am. J. Dis. Child. 1972, 123:254-258. 5. Kassner E.G. et al.: Am. J. Roentgenol. 1976, 127:927-933. 6. Weiss L. et al.: Frontometaphyseal dysplasia. Evidence for dominant inheritance. Am. J. Dis. Child. 1976, 130:259-261. 7. Medlar R.C., Crawford A.H.: Frontometaphyseal dysplasia. J. Bone Joint Surg. (Am) 1978, 60A:392-394. 8. Kanemura T. et al.: Frontometaphyseal dysplasia: Evidence for autosomal dominant inheritance). Am. J. Roentgenol. 1979, 127:927-933. 9. Gorlin R.J., Winter R.B.: Frontometaphyseal dysplasia – Evidence for X-linked inheritance. Am. J. Med. Genet. 1980, 5:81-84. 10. Fitzsimmons J.S. et al.: Frontometaphyseal dysplasia. Further delineation of the clinical syndrome. Clin. Genet. 1982, 22:195-205. 11. Park J.M. et al.: Mitral valve prolaps in a patient with frontometaphyseal dysplasia. Clin. Pediatr. (Phila) 1986, 25:469-471. 12. Spranger J.W. et al: Bone Dysplasias. Saunders Co. Philadelphia 1974, 321-322. 13. Beighton P., Cramin B.J.: Sclerosing Bone Dysplasias. Springer. Berlin 1980, 75-81. 14. Bieganski T., Makowski A.: Dysplasia czolowo-przynasadowa. Przegl. Radiol. 1995, 60:100-102. 15. Nishimura G. et al.: Radiological changes of frontometaphyseal dysplasia in the neonate. Ped. Radiol. 1995, 25:143-146.