Ostra niewydolność nerek w przebiegu przełomu hiperkalcemicznego u chorego z rakiem przytarczyc – opis przypadku
Acute renal failure in the course of hypercalcemic crisis due to parathyroid carcinoma – the case study
Department of Endocrinology, Centre of Postgraduate Medical Education, Bielański Hospital, Warszawa
Head of Department: prof. Wojciech Zgliczyński, MD, PhD
Parathyroid carcinoma is an uncommon cause of primary hyperparathyroidism. Approximately only 400 cases of this disease were reported in the English since 1930 (1-28). The clinical features of parathyroid carcinoma are due primarily to the effects of hypercalcaemia due to excessive PTH secretion and do not consist the typical features of advanced neoplastic disease (1-6, 9-10, 12, 18, 27-28). Thus, unlike in the majority of present-day benign primary hyperparathyroidism cases, signs and symptoms of acute hypercalcemia often dominate the clinical picture in parathyroid carcinoma, the controlling of which becomes, in consequence, the primary goal of the therapy. The critical, life-threatening hypercalcemia (hypercalcemic crisis) of parathyroid carcinoma is treated in the same way as hypercalcemia due to any other case (28-30). Due to the persistently excessive PTH secretion, saline hydration and loop diuretics rarely suffice to control the hypercalcemia, and addition of agents that interfere with osteoclast-mediated bone resorption is always necessary. However, in the case described here, the classic inhibitors of osteoclastic bone resorption, i.e. bisphosphonates, could not be used because of acute renal failure. Upon application the cinacalcet (Mimpara®, Amgen) – a calcimimetic, a drug of a new therapeutic class, a satisfactory reduction of calcemia was achieved.
A 56-year-old male was admitted to the hospital lethargic and fell asleep during examination. He also experienced intermittent nausea, vomiting, and watery diarrhea, however he denied having any fever, chills, or any other associated symptoms. He also noted excessive thirst and increased in urination but denied dysuria or hematuria. His past medical history was only significant for nephrolithiasis. He was not taking any medications regularly. However, he complained of worsening pain in the spine and pelvis and noted a painful deformation of the right knee and the lower leg. Physical examination revealed blood pressure of 160/80 mmHg, heart rate 96/min regular. His cardiopulmonary exam was unremarkable. Abdominal exam revealed mild tenderness in the epigastrium area and left lower quadrant without any signs of guarding or rigidity. Bowel sounds were active. Acute abdominal series X-ray did not show any acute process. Bedside glucose reading was 115 mg/dl. Laboratory investigation showed normal CBC and urine analysis. Serum creatinine level was 5.4 mg/dL (0.5-1.4 mg/dL). Serum calcium was 14.5 mg/dL (reference range 8-10.5 mg/dL), and ionized calcium was elevated at 1.78 mmol/L (reference range 1.10-1.30 mmol/L) and the acute renal failure in the course of hypercalcemic crisis was diagnosed.
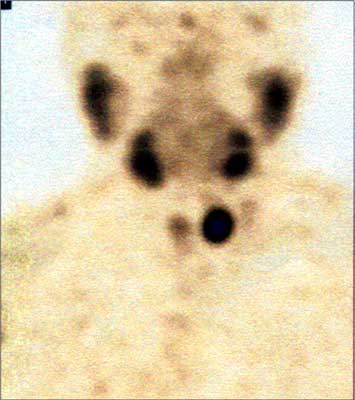
Patient was treated with intravenous fluid hydration and loop diuretic while the etiology of hypercalcemia was being sought. Extremely elevated serum PTH-intact level of 1789 pg/ml confirmed the diagnosis of primary hyperparathyroidism and a possibility of parathyroid carcinoma had been considered. Left knee and lower leg X-ray and CT revealed a typical picture of osteitis fibrosa cystica (fig. 1). Renal failure excluded the possibility of using the standard symptomatic treatment of hypercalcemia, which are bisphosphonates. Hydratation and furosemide treatment improved significantly renal function, however had a very little effect on serum calcium level. Eventually, it was decided to treat patient with calcimimetic – cinacalcet (Mimpara®), recently registered for symptomatic control of hypercalcemia due to primary hyperparathyroidism. After the administration of the drug at the smallest recommended dose of 30 mg twice a day, the serum calcium began to reduce at a quick rate, dropped to 12.24 mg/dL after the third day of the treatment, and after increase of total daily dose to 90 mg/d, subsequently deceased above 12.00 mg/dL. Consequently, the saline hydration was stopped, which in turn did not affect the serum calcium values. After two weeks of cinacalcet treatment the PTH levels also decreased from 1789 pg/ml before the start of the treatment to 785 pg/ml, respectively. Improving the general condition of the patient allowed to perform the parathyroid imagining studies. Technetium 99mTc-MIBI scan as well as computed tomography indicated the enlarged left inferior parathyroid gland (fig. 2). The patient underwent surgery. Enlarged parathyroid tumor (3.0 x 3.0 cm) had been removed with left thyroid lobe and isthmus, and with surrounding, not enlarged and macroscopically unaffected lymph nodes. The left reccurent laryngeal nerves was preserved with neuromonitoring use. Twenty-four hours after surgery, serum calcium was 6.8 mg/dL, phosphorus was 1.6 mg/dL, and PTH was 24 pg/ml, with subtetany symptoms and positive Chvostek’s sign. Patient had been treated with calcium gluconate iv and then with oral calcium carbonate (3.0 g daily) and alphacalcidiol up to 3.0 μg/daily. He was discharged two week later. Histopathological diagnosis of the parathyroid carcinoma had been established.
1. Holmes E, Morton D, Ketcham A: Parathyroid carcinoma: a collective review. Ann Surg 1969; 169: 631-640.
2. Schantz A, Castleman B: Parathyroid carcinoma: a study of 70 cases. Cancer 1973; 31: 600-605.
3. Shane E, Bilezikian J: Parathyroid carcinoma: a review of 62 patients. Endocr Rev 1982; 3: 218-226.
4. Cohn K, Silverman M, Corrado J et al.: Parathyroid carcinoma: The Lahey Clinic experience. Surgery 1985; 98: 1095-1110.
5. Wang C, Gaz R: Natural history of parathyroid carcinoma: diagnosis, treatment, and results. Am J Surg 1985; 149: 522-527.
6. Shane E, Bilezikian J: Parathyroid carcinoma. [In:] Williams CJ, Green MR, Raghaven D (eds.): Textbook of uncommon cancer. Wiley & Sons, New York 1987: 763-771.
7. Obara T, Fujimoto Y: Diagnosis and treatment of patients with parathyroid carcinoma: an update and review. World J Surg 1991; 15: 738-744.
8. Sandelin K, Thompson NW, Bondeson L: Metastatic parathyroid carcinoma: dilemmas in management. Surgery 1991; 110: 978-986.
9. Wynne A, Heerden Jv, Carney J et al.: Parathyroid carcinoma: clinical and pathological features in 43 patients. Medicine 1992; 71: 197-205.
10. Hakaim AG, Esselstyn CB Jr: Parathyroid carcinoma: 50-year experience at The Cleveland Clinic Foundation. Cleve Clin J Med 1993; 60: 331-335.
11. Obara T, Okamoto T, Ito Y et al.: Surgical and medical management of patients with pulmonary metastasis from parathyroid carcinoma. Surgery 1993; 114: 1040-1048.
12. Vetto JT, Brennan MF, Woodruf J et al.: Parathyroid carcinoma: diagnosis and clinical history. Surgery 1993; 114: 882-892.
13. Cryns VL, Rubio MP, Thor AD et al.: p53 abnormalities in human parathyroid carcinoma. J Clin Endocrinol Metab 1994; 78: 1320-1324.
14. de Papp AE, Kinder B, LiVolsi V et al.: Parathyroid carcinoma arising from parathyroid hyperplasia: autoinfarction following intravenous treatment with pamidronate. Am J Med 1994; 97: 399-400.
15. Rosen IB, Young JE, Archibald SD et al.: Parathyroid cancer: clinical variations and relationship to autotransplantation. Can J Surg 1994; 37: 465-469.
16. Martinez DA, King DR, Romshe C et al.: Intraoperative identification of parathyroid gland pathology: a new approach. J Pediatr Surg 1995; 30: 1306-1309.
17. Miki H, Sumitomo M, Inoue H et al.: Parathyroid carcinoma in patients with chronic renal failure on maintenance hemodialysis. Surgery 1996; 120: 897-901.
18. Mendoza V, Hernandez AF, Marquez ML et al.: Primary hyperparathyroidism due to parathyroid carcinoma. Arch Med Res 1997; 28: 303-306.
19. Vainas IG, Tsilikas C, Grecu A et al.: Metastatic parathyroid carcinoma (mPCa): natural history and treatment of a case. J Exp Clin Cancer Res 1997; 16: 429-432.
20. Chow E, Tsang RW, Brierley JD et al.: Parathyroid carcinoma – the Princess Margaret Hospital experience. Int J Radiat Oncol Biol Phys 1998; 41: 569-572.
21. Collins MT, Skarulis MC, Bilezikian JP et al.: Treatment of hypercalcemia secondary to parathyroid carcinoma with a novel calcimimetic agent. J Clin Endocrinol Metab 1998; 83: 1083-1088.
22. Cordeiro AC, Montenegro FL, Kulcsar MA et al.: Parathyroid carcinoma. Am J Surg 1998; 175: 52-55.
23. Favia G, Lumachi F, Polistina F et al.: Parathyroid carcinoma: sixteen new cases and suggestions for correct management. World J Surg 1998; 22: 1225-1230.
24. Yoshimoto K, Endo H, Tsuyuguchi M et al.: Familial isolated primary hyperparathyroidism with parathyroid carcinomas: clinical and molecular features. Clin Endocrinol (Oxf) 1998; 48: 67-72.
25. Boyle NH, Ogg CS, Hartley RB et al.: Parathyroid carcinoma secondary to prolonged hyperplasia in chronic renal failure and in coeliac disease. Eur J Surg Oncol 1999; 25: 100-103.
26. Bradwell AR, Harvey TC: Control of hypercalcaemia of parathyroid carcinoma by immunisation. Lancet 1999; 353: 370-373.
27. Hundahl SA, Fleming ID, Fremgen AM et al.: Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985-1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 1999; 86: 538-544.
28. Shane E: Parathyroid carcinoma. J Clin Endocrinol Metab 2001; 86: 485-493.
29. Bilezikian J: Management of acute hypercalcemia. N Engl J Med 1992; 326: 1196-1203.
30. Shane E: Hypercalcemia: pathogenesis, clinical manifestations, differential diagnosis and management. [In:] Favus M (ed.): ASBMR primer on metabolic bone disease. Ed. 4, Lippincott-Raven, Philadelphia 1999: 183-186.
31. Heath H, Hodgson S, Kennedy M: Primary hyperparathyroidism: incidence, morbidity, and potential economic impact in a community. N Engl J Med 1980; 302: 189-193.
32. Silverberg SJ, Shane E, de la Cruz L et al.: Skeletal disease in primary hyperparathyroidism. J Bone Miner Res 1989; 4: 283-291.
33. Bilezikian J, Silverberg S, Shane E: Primary hyperparathyroidism in the 1980’s. [In:] Kleerekoper MKS (ed.): Clinical disorders of bone and mineral metabolism. Mary Anne Liebert, New York 1989: 359-365.
34. Holck S, Pedersen N: Carcinoma of the parathyroid gland. A light and electron microscopic study. Acta Pathol Microbiol Scand 1981; 89: 297-302.
35. Smith J, Coombs R: Histological diagnosis of carcinoma of the parathyroid gland. J Clin Pathol 1984; 37: 1370-1378.
36. Fujimoto Y, Obara T, Ito Y et al.: Localization and surgical resection of metastatic parathyroid carcinoma. World J Surg 1986; 10: 539-547.
37. Johnston LB, Carroll MJ, Britton KE et al.: The accuracy of parathyroid gland localization in primary hyperparathyroidism using sestamibi radionuclide imaging. J Clin Endocrinol Metab 1996; 81: 346-352.
38. Obara T, Fujimoto Y, Tanaka R et al.: Mid-mediastinal parathyroid lesions: preoperative localization and surgical approach in two cases. Jpn J Surg 1990; 20: 481-486.
39. Calandra D, Chejfec G, Foy B et al.: Parathyroid carcinoma: Biochemical and pathologic response to DTIC. Surgery 1984; 96: 1132-1137.
40. Bukowski R, Sheeler L, Cunningham J et al.: Successful combination chemotherapy for metastatic parathyroid carcinoma. Arch Int Med 1984; 144: 399-400.
41. Chahinian A, Holland J, Nieburgs H et al.: Metastatic nonfunctioning parathyroid carcinoma: ultrastructural evidence of secretory granules and response to chemotherapy. Am J Med Sci 1981; 282: 80-84.
42. Sigurdsson G, Woodhouse N, Taylor S et al.: Stilboestrol diphosphate in hypercalcemia due to parathyroid carcinoma. Br Med J 1973; 1: 27-28.
43. Goepfert H, Smart C, Rochlin D: Metastatic parathyroid carcinoma and hormonal chemotherapy; case report and response to hexestrol. Ann Surg 1966; 164: 917-918.
44. Singer FR, Neer RM, Murray TM et al.: Mithramycin treatment of intractable hypercalcemia due to parathyroid carcinoma. N Engl J Med 1970; 283: 634-636.
45. Dubost C, Jehanno C, Lavergne A et al.: Successful resection of intrathoracic metastases from two patients with parathyroid carcinoma. World J Surg 1984; 8: 547-551.
46. Lake M, Kahn S, Favus M et al.: Case report: clinical pathological correlations in a case of primary parathyroid carcinoma. Ann Clin Lab Sci 1984; 14: 458-463.
47. Trigonis C, Cedermark B, Willems J et al.: Parathyroid carcinoma – Problems in diagnosis and treatment. Clin Oncol 1984; 10: 11-19.
48. Warrell R, Isaacs M, Alcock N et al.: Gallium nitrate for treatment of refractory hypercalcemia from parathyroid carcinoma. Ann Intern Med 1987; 197: 683-686.
49. Jungst D: Disodium clodronate is effective in management of severe hypercalcemia caused by parathyroid carcinoma. Lancet 1984; 1: 1043.
50. Jacobs T, Siris E, Bilezikian J et al.: Hypercalcemia of malignancy: treatment with intravenous dichloromethylene diphosphonate. Ann Intern Med 1981; 94: 312-316.
51. Shane E, Jacobs T, Siris E et al.: Therapy of hypercalcemia due to parathyroid carcinoma with intravenous dichloromethylene diphosphonate. Am J Med 1982; 72: 939-944.
52. Mann K: Oral bisphosphonate therapy in metastatic parathyroid carcinoma. Lancet 1985; 1: 101-102.
53. Sandelin K, Thompson N, Bondeson L: Metastatic parathyroid carcinoma: dilemmas in management. Surgery 1992; 110: 978-988.
54. Weinstein R: Parathyroid carcinoma associated with polycythemia vera. Bone 1991; 12: 237-239.
55. Chang JT, Green L, Beitz J: Renal Failure with the Use of Zoledronic Acid. N Engl J Med 2003; 349: 1676-1679.
56. Brown EM: Calcium receptor and regulation of parathyroid hormone secretion. Rev Endocrinol Metab Dis 2000; 1: 307-315.
57. Nemeth EF, Fox J: Calcimimetic compounds; a direct approach to controlling plasma levels of parathyroid hormone in hyperparathyroidism. Trends Endocrinol Metab 1999; 10: 66-71.
58. Nemeth EF, Heaton WM, Miller M et al.: Pharmacodynamics if the type II calcimimetic compound cinacalcet HCl. J Pharmacol Exp Ther 2002; 308: 627-635.
59. Silverberg SJ, Bone III HG, Marriott TB et al.: Short-term inhibition of parathyroid hormone secretion by a calcium – receptor agonist in patients with primary hyperparathyroidism. N Engl J Med 1997; 337: 1506-1510.
60. Silverberg SJ, Faiman C, Bilezikian JP et al.: The effects of Cinacalcet HCl (AMG 073) on serum calcium levels in patients with parathyroid carcinoma or recurrent primary hyperparathyroidism after parathyroidectomy. 26th Annual Meeting of the ASBMR 2004; Abstract SA 420.
61. Silverberg SJ, Faiman C, Bilezikian JP et al.: Cinacalcet HCl effectively treats hypercalcemia in patients with parathyroid carcinoma. 25th Annual Meeting of the ASBMR 2003; Abstract SA 495.
62. Rubin MR, Sliney J, Silverberg SJ et al.: Clinical Course of 10 Patients with Inoperable Parathyroid Carcinoma Treated with the Calcimimetic Cinacalcet HCl. 26th Annual Meeting of the ASBMR 2004; Abstract SA 497.
63. Peacock M, Bilezikian JP, Klassen PS et al.: Cinacalcet hydrochloride maintains long-term normocalcemia in patients with primary hyperparathyroidism. J Clin Endocrinol Metab 2005; 90: 135-141.