© Borgis - New Medicine 4/2014, s. 122-125
Teresa Ryczer, *Lidia Zawadzka-Głos
A rare case of Burkitt’s lymphoma in paranasal sinuses in a child
Department of Pediatric Otolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Summary
Introduction. Burkitt’s lymphoma is a malignant tumor of lymphatic system that originates from B lymphocytes in germinal center of lymph nodes. There may be different clinical types of Burkitt’s lymphoma. Clinical manifestation of disease can involve different localization.
Aim. The aim of the study is to present a rare case of a 4.5-year-old patient With Burkitt’s lymphoma of craniofacial localization with paranasal sunus involvement.
Material and methods. The patient with Burkitt’s lymphoma was hospitalized in the Department of Pediatric Otolaryngology of Medical University of Warsaw in may 2013. Signs and symptoms, results of diagnostic examinations and treatment will be discussed. Available medical record of the patient and diagnostic images were used to prepare the case report.
Results. A 4.5-year-old male patient was admitted to the Pediatric ENT Department due to painless swelling and erythema of the right cheek that persisted for a week. ENT examination revealed edema and erythema of the right cheek, neck lymphadenopathy with no other abnormalities. CT of paranasal sinuses showed vast, soft-tissued mass in the right maxillary sinus, with no contrast enhancement, infiltrating orbita, optic nerve, pterygopalatine fossa. The result of the biopsy was Burkitt’s lymphoma.
Conclusions. Malignant tumors of head and neck in children are rare. First symptoms of Burkitt’s lymphoma may be localized in craniofacial area, thus, especially general practicioners and pediatricians should be aware of careful diagnostic procedures and treatment in these patients. Computed tomography with contrast should be performed in case of any non-specific anomaly in head area. Chemotherapy is treatment of choice in Burkitt’s lymphoma.
INTRODUCTION
Burkitt’s lymphoma (BL) is recognized as a highly malignant B-cell non-Hodgkin’s lymphoma. Burkitt’s lymphoma can be divided into three main clinical types: endemic, sporadic and immunodeficiency-associated. The endemic variant, also known as African variant, occurs mainly in children living in malaria endemic regions of the world, e.g. equatorial Africa, Brazil, Papua New Guinea. In almost all patients with endemic variant of BL Epstein-Barr Virus is found. The disease involves jaw or other facial bones, ileum, cecum, ovaries, kidneys or mediastinum. The sporadic type („non-African”, or „American”) is the most common one in places where malaria is not endemic. In this type of Burkitt’s lymphoma EBV association is rare. The sporadic Burkitt’s lymphoma involves mainly ileocecal region, and rarely involves orbit or paranasal sinuses. Immunodeficiency-associated Burkitt lymphoma occurs usually in immunocompromised patients with HIV infection or after organ transplantation (1, 2). All types of BL are histologically comparable with the difference of epidemic presentation. Symptoms of Burkiit’s lymphoma may be various, thus diagnostic procedures depend on signs and symptoms presented by patient. Burkitt’s lymphoma treatment consist of chemotherapy. Other therapy may be immunotherapy, bone marrow transplants, stem cell transplant, surgery to remove tumor, and radiotherapy.
METHODS
We would like to present a rare case of a 4.5-year-old patient with Burkitt’s lymphoma of craniofacial localization as first symptom that was hospitalized in the Department of Pediatric Otolaryngology of Medical University of Warsaw in may 2013. Signs and symptoms, results of diagnostic examinations, treatment and follow-up will be discussed.
RESULTS
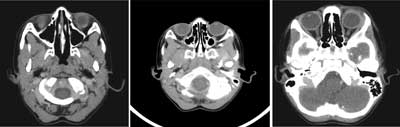
A 4.5-year-old male patient was admitted to the Pediatric ENT Department due to painless swelling and erythema of the right cheek for a week. In ENT examination there was edema and erythema of the right cheek, neck lymphadenopathy, with no other abnormalities. The patient otherwise appeared normal, with no symptoms of proptosis, epistaxis, headache, fever, weight loss, or night sweats. There was no clinical improvement to applied antibiotic therapy which consisted of clindamycin and cefuroxim. Ultrasonography of the cheek showed hyperechogenic, hyperemic area within soft tissues of the cheek with irregular fluid spaces, and enlarged lymph nodes within the right parotid gland and in the neck. CT scan revealed vast, soft-tissued mass in the right maxillary sinus, with no specific contrast enhancement, infiltrating soft tissues of the orbita, optic nerve, pterygopalatine fossa, masticatory and temporal muscle, buccal space and showed destruction of bony elements of maxillar sinus, as well as of ala mayor of sphenoid sinus (fig. 1).

Fig. 1. CT scan of paranasal sinuses revealed vast, soft-tissued mass in the right maxillary sinus, with no specific contrast enhancement, infiltrating soft tissues of the orbita, optic nerve, pterygopalatine fossa, masticatory and temporal muscle, buccal space and showing destruction of bony elements of maxillar sinus, as well as of ala mayor of sphenoid sinus.
The biopsy of the lesion under general anesthesia was performed. First, the biopsy of the cheek lesion, and afterwards the biopsy of a mass in maxillary sinus through inferior antrostomy was done. At the same time, bone marrow biopsy was performed. The result of the surgical biopsy revealed Burkitt’s lymphoma. Bone marrow biopsy showed no abnormalities in myelogram. The patient was transferred to the Department of Hematology and Oncology for further diagnostic procedures and treatment. There were no signs of pancythopenia in blood test, LDH was normal. Examination of the cerebrospinal fluid did not show any atypical cells.
On neurological consultation asynchronous movements of the eye balls (the right eye ball was slightly slower) and a slight asymmetry of pupills (the right one was slightly narrower than the left one) were stated. Other CT scans were planned in order to assess clinical staging of the disease. Computed tomography showed pathological hypodense mass in mediastinum in the area of cervical vessels, size 23 x 35 x 30 mm and enlarged lymph node in the left axillary fossa, size 11 x 7 mm. CT of abdomen revealed abnormal hypodense mass within the head of pancreas, size 27 x 24 mm, and enlarged liver with two hypodense small lesions in the right lobe and one lesion in the left lobe, all around 6 mm of size. Stage IV Burkitt’s lymphoma was diagnosed. The patient underwent multidrug chemotherapy according to protocol EICNHL-COG InterBNHL 2010 group C. After 2 months CT scan was performed, that showed regression of the tumor in craniofacial area, only small lesions in the right maxillary sinus were described. There was also regression of the tumor in abdomen, however, there was no regression of the mass in mediastinum. In consequence, in september 2014 the patient underwent surgery of the mediastinal tumor in Thoracic Surgery Department. Histopathological examination of the removed tumor tissue showed lymhangioma cavernosum, with no signs of Burkitt’s lymphoma involvement. After 6 months CT scan of sinuses showed remnant tissues in pterygopalatine fossa, size 11 x 4 mm and 7 x 4 mm, and slightly thickened mucosa of the maxillary sinuses walls, with no other abnormalities (fig. 2). Follow-up after 6 months showed remision of Burkitt’s lymphoma. We do not have up-to-date data about further follow-up due to the fact that the patient and his family moved to Portugal.
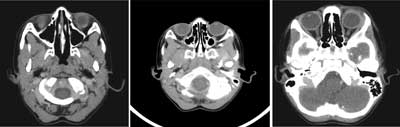
Fig. 2. CT of paranasal sinuses after chemotherapy showed regresion of tumor masses in maxillary sinus, in orbita area and within optic nerve. The only abnormalities revealed on CT were remnants of tissue in pterygopalatine fossa, size 11 x 4 mm and 7 x 4 mm, and slightly thickened mucosa of the maxillary sinuses walls.
DISCUSSION
Only about 5% to 10% of primary malignant conditions in the pediatric group originate in the head and neck. Non-Hodgkin’s lymphoma has an occurrence rate of about 26% in pediatric head and neck malignancies. It was first reported in 1958 by a British missionary surgeon, Sir Dennis Burkitt, who described a multifocal tumor syndrome that involved expansion of the jaws accompanied by loosening and irregular displacement of teeth in Ugandan children (5). Clinically, jaw and midfacial lesions appear to dominate the endemic forms of the disease whereas abdominal (ileocecal) involvement is seen in the sporadic type (1-5). Most of endemic types of BL are associated with EBV infection, on the other hand, less than 15% of sporadic BL contains EBV DNA material (4).
In the head and neck area, Burkitt’s lymphoma frequently involves the cervical lymph nodes. In less than a quarter of the reported cases, Burkitt’s lymphoma appeared in the extranodal region of the head and neck area. The paranasal localisation of BL is extremely rare. In a study of 196 Nigerian children with BL, 66% had involvement of the jaw and 12% had involvement of the paranasal sinuses (3). If the tumor is in the abdomen, it often leads to nausea, vomiting, and pain, due to the intestinal obstruction. The diagnosis of Burkitt’s lymphoma, especially when the primary symptom is in the oral and maxillofacial region, is often difficult because of the wide variety of presenting signs and symptoms. The clinical symptoms of Burkitt’s lymphoma in the head and neck region strongly depend on the anatomic site of its involvement. If the tumor is in the head and neck region, the patient may have symptoms of nasal obstruction, rhinorrhea, facial swelling, ophthalmic involvement, tonsillar enlargement, and cervical lymphadenopathy. This problem can easily be misdiagnosed as nasal polyposis or acute or chronic sinusitis (1, 2). In the early stage, therefore, Burkitt’s lymphoma can be treated incorrectly as an upper airway infection or other inflammatory diseases.
Most cases occur in patients younger than 10 years of age (2). The mean age of involvement in endemic BL is 7 years and in sporadic BL is 11 (2). There is a peak incidence between ages 5 and 7 years (4). Both endemic and sporadic types affect twice as many boys as girls (4). Our patient was 4.5-year-old white boy.
Sinus involvement is most frequently maxillary and then sphenoidal and ethmoidal (2). In case of presented patient the BL localization was mainly the right maxillary sinus with involvement of orbital and pterygopalatine fossa. In the cases of BL nasopharyngeal involvement, the patients may also have otitis media (1). Although extremely rare in the sporadic variety, BL has been described, apart from the nasopharynx, also in cavernous sinus (3). The most common malignancy involving the paranasal sinuses is squamous cell carcinoma (SCC). Differential diagnosis of BL should include lesions such as SCC, ossifying fibroma, osteosarcoma, Langerhans cell disease, giant cell tumor, salivary gland tumors, including mucoepidermoid carcinoma and fibrous dysplasia (2, 4).
Fine needle aspiration is generally inadequate for the diagnosis, because it usually yields only small-cell lymphocytes without adequate information about the tissue architecture to characterize the case further. Open biopsy is necessary to obtain adequate tissue for appropriate immunohistochemical studies. Imaging procedure such as computed tomography and magnetic resonance imaging can help determine the extent of the primary disease, and a total body disease workup should include positron emission tomography and evaluation of the bone marrow and cerebrospinal fluid (2). Our patient had open biopsy of the cheek lesion and subsequently the biopsy of the mass in maxillar sinus. He underwent CT scans of head and neck, mediastinum and abdomen. He had also PET imaging, that after 4-months of therapy showed metabolically active tumor-like lesion in mediastinum. Afterwards, the patients was refered to undergo surgical treatment of the mediastinal tumor, which ocurred to be lymphangioma cavernosum according to histopathological assessment.
Associated with a cell doubling time of 24 to 26 hours, BL ranks among the fastest growing of all human tumors and needs prompt intervention. The tumor grows very rapidly and spreads by blood dissemination. The primary therapeutic modality for BL is chemotherapy. Early diagnosis before the dissemination and prompt initiation of chemotherapy are the keys for good prognosis (1, 2). As our follow-up results demonstrated, our patient with stage IV Burkitt’s lymphoma had a good response to chemotherapy. When patients are treated with the traditional regimen, the prognosis of Burkitt’s lymphoma is very good with a 85% to 95% 5-year event-free survival (EFS) rate (1, 4). The findings of EBV antibodies is of no clinical importance, just for scientifical interest, because the protocol of management for both endemic and sporadic BL types is the same (4).
CONCLUSIONS
Malignant tumors of head and neck in children are rare. Primary symptoms of Burkitt’s lymphoma can be localized in craniofacial region. Paranasal sinuses are extremely rare BL involvement. Thus, especially general practicioners and pediatricians should be aware of careful diagnostic procedures and treatment in these patients. Any abnormal non-specific mass in the craniofacial area should be consulted with the ENT specialist. Computed tomography with contrast should be performed in case of any non-specific anomaly in head area. Chemotherapy is treatment of choice in Burkitt’s lymphoma.
Piśmiennictwo
1. Chen DT, Chen PR, Hsu LP et al.: Burkitt’s lymphoma in paranasal sinuses. Otolaryngol Head Neck Surg 2006; 135: 991-993. 2. Nikgoo A, Mirafshariyeh SA, Kazeminajad B et al.: Burkitt’s Lymphoma of Maxillary Sinuses: Review of Literature and Report of Bilateral Case. J Oral Maxillofac Surg 2009; 67: 1755-1763. 3. Pereira KD, Smith Stacey L: Sporadic Burkitt’s lymphoma masquerading as an orbital complication of sinusitis. Int J Pediatr Otorhinolaryngol Extra 2006; 1: 315-318. 4. Lund DI, Rodd H, Craig GT: Burkitt’s lymphoma presenting with jaw lesions in a young white girl. J Oral Maxillofac Surg 1997; 35: 438-441. 5. Nissenbaum M, Kaban LB, Troulis MJ: Toothache, Paresthesia and Horner Syndrome: An Unusual Presentation of Disseminated Burkitt’s Lymphoma. J Oral Maxillofac Surg 2007; 65: 1395-1401. 6. Gaini RM, Romagnolia M, Sala A, Garavelloa W: Lymphomas of head and neck in pediatric patients. Int J Pediatr Otorhinolaryngol 2009; 73S: S65-S70. 7. Roh JL, Huh J, Moon HN: Lymphomas of the head and neck in the pediatric population. Int J Pediatr Otorhinolaryngol 2007; 71: 1471-1477. 8. Weisberger EC, Davidson DD: Unusual presentations of lymphoma of the head and neck in childhood. Laryngoscope 1990; 100: 337-342. 9. Bauer GP, Volks MS, Siddiqui SY et al.: Burkitt’s lymphoma of the parafaryngeal space. Arch Otolaryngol Head Neck Surg 1993; 119: 117-120. 10. Vasconcelos Seixasa D, Lobob AL, Farinhab NJ et al: Burkitt leukemia with numb chin syndrome and cavernous sinus involvement. Eur J Pediatr Neurol 2006; 10: 145-147. 11. Mawardi H, Cutler C, Treister N: Medical management update: Non-Hodgkin lymphoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: e19-e33. 12. Wang M, Strasnick B, Zimmerman MC et al.: Extranodal American Burkitt’s lymphoma of the head and neck. Arch Otol Head Neck Surg 1992; 118: 193-199. 13. Banthia V, Jen A, Kacker A et al.: Sporadic Burkitt’s lymphoma of the head and neck in the pediatric population. Int J Pediatr Otorhinolaryngol 2003; 67: 59-65. 14. Jan A, Vora K, Sandor GKB: Sporadic Burkitt’s lymphoma of the jaws: The essentials of prompt life-saving referral and management. J Can Dent Assoc 2005; 71: 165. 15. Otmani N, Khattab M: Oral Burkitt’s lymphoma in children: The Moroccan experience. Int J Oral Maxillofac Surg 2008; 37: 36.