© Borgis - New Medicine 4/2014, s. 133-135
Monika Jabłońska-Jesionowska, Małgorzata Dębska, Renata Koziołek, *Lidia Zawadzka-Głos
Congenital absence of the right pulmonary artery rare casuse of radiological changes suggestive of bronchial foreign body
Department of Pediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head of Department: Lidia Zawadzka-Głos, MD, PhD
Summary
We report the case of 6.5 year old girl admitted to the Department of Pediatric ENT in Warsaw Medical University in January 2013 suspected of the foreign body in the right bronchus because of the characteristic signs on chest X-ray: emphysema, mediastinal shift to the right, athelectasis and asymmetrical respiratory murmur, weakened on the right. She was investigeted because of persisting cough for more than 3 weeks after infection. The child was qualified for urgent bronchoscopy. The procedure was performed under general anaesthesia using the rigid bronchoscop No. 5. Neither pathology of the respiratory tract nor foreign bodies were found. The further investigation CT scan of the chest shows the absence of the right pulmonary artery. Congenital absence of a right pulmonary artery is a rare abnormality of great vessels. The lack of the right pulmonary artery are often asymptomatic. The abnormal chest X-ray suggesting bronchial foreign body with normal result of bronchoscopy at the same time led to further investigations.
INTRODUCTION
A bronchial foreign bodies are a common cause of hospitalization of children on the ENT wards. The common symptoms of a foreign bodies aspiration depends on the type of foreign body and its location. Shortness of breath with respiratory stridor after an episode of choking is an absolute indication for urgent bronchoscopy under general anaesthesia. Chronic cough persisting after treatment of respiratory infections, recurrent bronchitis at the same parts of the lung and characteristic findings in the chest x-ray are also indications for bronchoscopy. Same foreign bodies are already visible on X-ray. Non-visible foreign bodies may appear on radiogram as: emphysema, athelectasis, mediastinal shift. The chest physical examination shows asymmetrical and weakened respiratory murmur, excessive tapping noise and wheeziness. Only performing the bronchoscopy can confirm or exclude the retention of a foreign body in the airways with possibility of evacuation.
CASE REPORT
A 6.5 year old girl was admitted to the Department of Pediatric ENT at Warsaw Medical University in January 2013 from the district hospital suspected of the foreign body in the right bronchus. In an interview: a month ago she has a respiratory tract infection with elevated body temperature, runny nose, cough, treated with an antibiotic. Because of the persisting cough for more than three weeks family doctor ordered chest X-ray examination. The results were as followed: hyperventilation of the left lung, mediastinal shift to the right, atelectasis of the right lung. There was no previous episode of choking. The girl was generally good health, growing up according to her age, attending kindergarten. At the admission to the hospital the auscultation shows: asymmetry of the respiratory murmur, weakened on the right side. In laboratory tests (complete blood count, ESR, CRP), there was no deviation from the norm. The child was qualified for urgent bronchoscopy. The procedure was performed under general anaesthesia using the rigid bronchoscop No. 5. Neither pathology of the respiratory tract nor foreign bodies were found. Only a small amount of mucous secretions was sucked for bacteriological examination. After 18 hours of inspection control chest x-ray was performed with the same results: hyperventilation of the left lung, a shift of the mediastinal structures to the right side, atelectasis of the right lung (fig. 1).
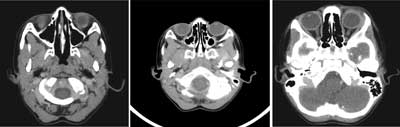
Fig. 1. Chest X-ray: the hyperventilation of the left lung, mediastinal shift to the right.
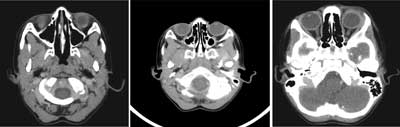
The physical examination changes were as before. Chest computed tomography (CT) was performed in accordance with the suggestion of radiologist. The results of CT scan of the chest were: the absence of the right pulmonary artery (fig. 2), the right lung vasculaturization by MAPCA from the aorta, subclavian artery and right internal thoracic artery (fig. 3). Right lung volume reduced (fig. 4), mediastinal shift to the right side.

Fig. 2. The absence of the right pulmonary artery.

Fig. 3. The additional vessels (collaterals, MAPCA).

Fig. 4. Right lung volume reduced.
The child was referred to a pulmonologist. The electrocardiogram was taken and no changes were found and echocardiogram confirmed lack of the right pulmonary artery. The pulmonary hypertension was not confirmed. The Streptococcus viridans was grown from the secretion of the respiratory tract. The serological examinations of the previous respiratory infections revealed Parainfluenza positive IgG. One week after cough subsided. The girl needs constant cardiac and periodic pulmonary care.
DISCUSSION
Congenital absence of a pulmonary artery is a rare abnormality of great vessels – 0.39% of all congenital heart defects (2). The absence of the right pulmonary artery is usually an isolated abnormality (2), while a congenital lack of the left pulmonary artery is associated with the heart anomalies like: tetralogy of Fallot, right aortic arch, patent ductus arteriosus (2). The absence of the left pulmonary artery due to heart failure is usually diagnosed in early childhood, but the absence of the right pulmonary artery is not recognized due to a lack of any characteristic clinical symptoms. Vascularization of the lung in the absence of the right pulmonary artery goes from the additional vessels (collaterals, MAPCA) leaving the aortic arch and from intrabronchial or intercostal artery (3). The symptoms of congenital absence of the right pulmonary artery include: recurrent lower respiratory tract infections, reduced exercise tolerance, dyspnea during exertion, hemoptysis (1-3). 15% of patients are completely asymptomatic. During normal growth of the embryogenesis after formation of pulmonary arteries, vascularization of the lung derived from the aorta gradually disappears. In this case study this abnormal arteries may even increase, causing hemoptysis. According to the literature, approximately 20% of patients present that symptom (1, 3). In some cases the pulmonary hypertension appeared (25% of patients). During the diagnosis the chest x-ray is performed, in which the shift of the mediastinum structures to the side of the lack of pulmonary artery, reducing the intercostal space and hyperinflation of the lung on the opposite side is observed (3, 4). There are also signs suggesting a bronchial foreign body. Examinations which confirm the diagnosis is chest CT scans or MRI showing the anatomy of the current pulmonary artery and additional vessels (MAPCA) (1, 3). Patients remain under the constant cardiac and periodic pulmonary care. Over the life time pulmonary hypertension may developed, there is a risk of extensive bleeding and acute high altitude pulmonary edema. Early diagnosis can prevent serious complications, even death during delivery or high-altitude excursions (1). Described patient was rather asymptomatic, without frequent infections and without limitation in physical capacity during exercises. Only abnormal chest X-ray suggesting bronchial foreign body with normal result of bronchoscopy at the same time led to further investigations.
CONCLUSIONS
1. Radiological change on the chest X-ray in the nature atelectasis, emphysema ventilated, mediastinal shift of the structures is an indication for bronchoscopy.
2. It is imperative to perform a control chest X-ray the 1 day after bronchoscopy.
3. Persistent radiographic changes after bronchoscopy require further investigation.
4. Congenital abnormalities of the great vessels are a interdisciplinary problem and are often identified incidentally and in every age of the child.
5. Correct diagnosis can prevent life-threatening consequences.
Piśmiennictwo
1. Ten Harkel AD, Blom NA, Ottenkamp J: Isolated unilateral absence of pulmonary artery: a case report and review of the literature. Chest 2002; 122: 1471-1477. 2. Zyła-Frycz M, Kusa J, Kurek T et al.: Jednostronny wrodzony brak tętnicy płucnej – obraz kliniczny, możliwości diagnostyczne i terapeutyczne w oparciu o materiał własny. Kardiochir Torakochi Polska 2009; 6(1): 29-33. 3. Varun M, Bishav M, Gurpreet SW: Case report of isolated congenital absence of right pulmonary artery with collaterals from coronary circulation. Indian Heart J 2014; 66(2): 220-222. 4. Kumar Sighi A, Francis E, Krisha R: Isolated absence of right pulmonary artery. Ann Ped Cardiology. 5. Weber J, Ramili JL, London R et al.: Unilateral absence of a pulmonary artery. Chest 1983; 84: 729-732. 6. Morales P, Miravet L, Marco V: Agenesis of the right pulmonary artery in young asymptomatic girl. Eur Respir J 1991; 4: 1301-1302. 7. Herraiz SI, Perez GW, Vergara RF et al.: Unilateral agenesis of the pulmonary artery: experience with 4 cases. An Esp Pediatr 1993; 38: 139-144. 8. Serino W, Argento G, Fiorilli R et al.: The isolated agenesis of a branch of the pulmonary artery: a case report. Its diagnosis and therapy. Cardiologia 1993; 38: 531-534.