© Borgis - New Medicine 2/2013, s. 39-43
*Witold Woźniak1, R. Krzysztof Mlosek2, Grzegorz Górski1, Tomasz Miłek1, Piotr Zydlewski1, Piotr Myrcha1, Piotr Ciostek1
Endovascular treatment of iliac artery occlusion
1First Department and Clinic of General and Vascular Surgery of the Second Faculty of Medicine, Medical University of Warsaw, Poland
Head of Department: prof. Piotr Ciostek, MD, PhD
2Department of Ultrasound Diagnostics and Mammography of the Second Faculty of Medicine, Medical University of Warsaw, Poland
Head of Department: prof. Wiesław Jakubowski, MD, PhD
Summary
Aim. The objective of the study was to analyze the results of endovascular treatment of iliac artery occlusion depending on the type of atherosclerotic lesions according to the TASC II classification.
Materials and methods. 46 patients with occlusion of the common iliac arteries and/or external arteries were operated in our clinic from 2008 to 2012. Based on the angio CT/angiogram results, the changes have been classified as type B (20), C (16) and D (10) according to the TASC II classification. The group included 37 male and 9 female aged 41-85 years, mean age 66.15ys.
Results. Following successful percutaneous iliac artery angioplasty stent was implanted in 37 patients, whilst in 9 cases no stent was applied. Significant complications were observed in five patients: unstable coronary heart disease - 1 case, pseudoaneurysm of femoral artery 1 case, peripheral arterial embolism- 2 cases. A case of iatrogenic external iliac artery rupture with haemorrhage into the retroperitoneal space was noted. This patient required open surgery. All patients have been followed up to one year. At that time primary assisted patency was noted to be 100%.
Conclusions. 1. All TASC types of chronic iliac artery occlusion can be successfully managed using intravascular methods, with acceptable complication and conversion to open surgery rate. 2. Midterm results (annual primary assisted patency) have been very satisfactory. 3. Long-term patency of iliac artery angioplasty still require further investigation.
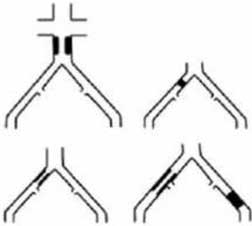
Technological progress of endovascular surgery, growing experience of centres using this method changed clinical indications to these operations. Advanced cases of lower limb atherosclerosis can be more successfully treated endovascularily. Previously, only cases of arterial stenosis were qualified for endovascular procedures, while currently angioplasty is increasingly used in patients with occlusion of lengthy arterial segments. Changes located in the aorto-iliac segment represent about 30% of lower limb atherosclerosis (1). Consensus TASC II (Trans Atlantic Inter-Society Consensus II) divides atherosclerotic lesions in this segment into four groups A, B, C and D. This classification takes into account the morphology and degree of atherosclerotic changes in the aorta and the iliac arteries (tab. 1). According to TASC II guidelines, endovascular method is a treatment of choice for group A. Group D lesions are scheduled routinely for classic aorto-iliac/femoral by pass surgery. Groups B and C are considered intermediate, both methods can be used. In group B intravascular method is preferred, whilst in Group C rather classic operation (2, 3). Based on these recommendations, major part of patients with aorto-iliac arterial occlusion should be operated in a classic manner. Aorto-ilio-femoral bypass is extensive surgical procedure and therefore risk of major postoperative complications is significant. On the other hand, endovascular treatment of iliac artery occlusion, if only feasible, is relatively safe and appears encouraging.
Table 1. The TASC II classification of atherosclerotic lesions in the aorto-iliac segment.
Type A Lesions
– Unilateral or Bilateral Stenoses of CIA
– Unilateral or Bilateral Single Short (≤ 3 cm) Stenosis of EIA |  |
Type B Lesions
– Short (≤ 3 cm) Stenosis of Infrarenal Aorta
– Unilateral CIA Occlusion
– Single or Multiple Stenosis Totaling 3-10 cm Involving the EIA Not Extending Into the CFA
– Unilateral EIA Occlusion Not Involving the Origins of Internal Iliac Or CFA | 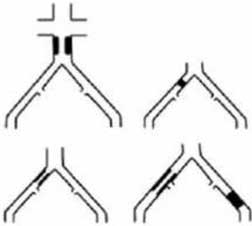 |
Type C Lesions
– Bilateral CIA Occlusions
– Bilateral EIA Stenosis 3-10cm Long Not Extending Into the CFA
– Unilateral EIA Stenosis Extending Into the CFA
– Unilateral EIA Occlusions That Involves the Origins of Internal Iliac and/or CFA
– Heavity Calcified Unilateral EIA Occlusion With Or Without Involvement of Origins of Internal Iliac and/or CFA |  |
Type D Lesions
– Infra-renal Aortoiliac Occlusion
– Diffuse Disease Involving the Aorta and Both Iliac Arteries Requiring Treatment
– Diffuse Multiple Stenoses Involving the Unilateral CIA, EIA, and CFA
– Unilateral Occlusions of both CFA and EIA
– Bilateral Occlusions of EIA Iliac Stenoses in Patients with AAA Requiring Treatment and Not Amenable of Endograft Placement or Other Lesions
– Requiring Open Aortic or Iliac Surgery | 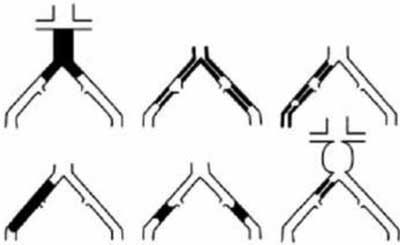 |
AIM
This study aimed to analyze the results of endovascular treatment of iliac artery occlusion in different TASC II types of atherosclerotic lesions.
MATERIALS AND METHODS
From 2008 to 2012, 46 patients with the occlusion of the common iliac arteries and/or external arteries were operated in our clinic. The group included 37 male and 9 female, aged 41-85 years, mean age 66.15 ys. The basic data of patients have been presented in table 2. The predominant clinical symptoms included intermittent claudication at distance below 100m, rest pain and tissue damage-toe/forefoot necrosis. The indications for surgery have been determined based on a physical examination and the imaging tests (ultrasound, computed tomography angiography). The patients with limb ischemia at the stages IIB, III and IV according to Fontaine were qualified for endovascular surgery. Based on angio CT/angiogram results, and according to TASC II classification, cases have been classified as type B (20), C (16) and D (10). Lower limb angiogram was performed via contralateral common femoral (30 cases) or axillary (12 cases) artery access. In four cases ipsilateral antegrade femoral artery access has been established. The procedure required local anaesthesia with 1% Xylocaine. A diagnostic catheter was inserted into the distal segment of abdominal aorta. Then, localisation and degree of arterial stenosis could be precisely analyzed. Arterial occlusion was negotiated by subintimal dissection with Terumo guidewire. Standard loop technique was performed. Then intraluminal re-entry was completed and confirmed on angiogram. At this stage any arterial perforation/extravasation was excluded. Then unfractioned heparin at a dose of 0.5 mg/kg of the body weight was administered intravenously. Angioplasty was performed using balloon catheters 7-10 mm in a diameter and 40-100 mm long. Final result was evaluated by control angiography. In case of residual stenosis or dissection of the iliac artery, a stent was implanted. Following surgery low molecular weight heparin was administered for 72 hours. Clopidogrel antiplatelet therapy (75 mg o.d.) administered for 3-6 months, was afterwards replaced by acetylsalicylic acid. The clinical result was assessed based on regression of pain, distance of intermittent claudication and rate of healing of trophic lesions. A follow up ultrasound was carried out at 1, 6 and 12 months post angioplasty. In case of doubt computerized tomography angiography was performed.
Table 2. The basic clinical data of patients qualified for endovascular treatment of iliac artery occlusion.
| | Number of patients | Percentage |
| Male | 37 | 80.4% |
| Female | 9 | 19.6% |
| Diabetes | 9 | 19.6% |
| Hypertension | 35 | 76.1% |
| Ischemic heart disease | 24 | 52.8% |
| Hyperlipidemia | 28 | 60.9% |
| Smoking | 37 | 80.4% |
| Claudication | 22 | 47.8% |
| Rest pain | 16 | 34.8% |
| Tissue necrosis | 8 | 17.4% |
| TASC B | 20 | 43.5% |
| TASC C | 16 | 34.8% |
| TASC D | 10 | 21.7% |
RESULTS
All 46 iliac artery occlusions have been successfully negotiated. 37 patients underwent iliac artery angioplasty with stent placement, in 9 patients no stent was applied. Right-sided iliac angioplasty was performed in 19 cases, while in 27 cases it was left-sided. Additionally, angioplasty of the superficial femoral artery and/or the popliteal artery was performed in 4 patients. According to TASC II, results were as follows.
In group B (20), common iliac artery angioplasty was performed in 12 patients, and external iliac artery was balooned in 8 patients. Following recanalization, iliac artery balloon angioplasty alone was performed in 7 cases and in the remaining 13 a stent was implanted. Complications were noted in two patients. Exacerbation of coronary heart disease – one patient, successfully treated pharmacologically. The other case was blue toe syndrome reported on operated side. Symptoms subsided spontaneously.
In group C (16), all patients underwent angioplasty of distal segment of the common iliac artery and proximal segment of external iliac artery. 8 patients required stent. Out of them, in 3 cases problems with re-entry were encountered. In these all cases the proper intraluminal channel was finally entered and angioplasty using a stent was completed. Two major complications have been noted in this group. Common femoral artery pseudoaneurysm at arterial access site was successfully treated with an ultrasound-guided injection of thrombin. The other case was acute ischemia of the operated limb, on the first day following angioplasty. It was caused by thrombosis of the superficial femoral popliteal arteries. Following angiography, local catheter directed thrombolysis was applied using the recombinant plasminogen activator for 24-hour period. Control angiogram showed no haemodynamically significant stenosis and therefore embolization was recognized a cause of ischemia. Clinical result was also satisfactory.
In group D (10), the long segments of common and external iliac arteries were re-canalized and stents were implanted in all cases. In one case re-entry problem resulted in external iliac artery rupture, causing haemorrhage into retroperitoneal space. The site of damage could not be treated using the intravascular method. A damaged artery was sutured, and the extent of atherosclerotic lesions necessitated ilio-femoral bypass. Further course of this patient treatment was uneventful.
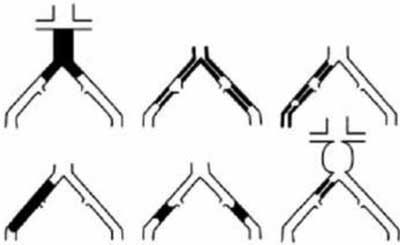
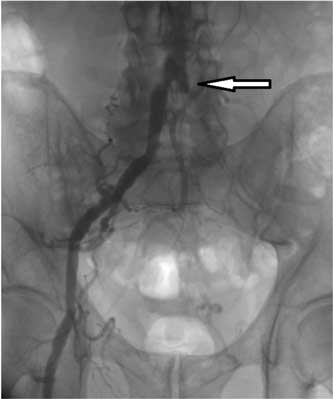
The aim of angioplasty was achieved in all patients. Improvement in clinical and hemodynamic parameters was noted. (fig. 1-3) There were no deaths no amputations. Ultrasound examinations performed 1 and 6 months post endovascular procedure, revealed patent iliac arteries. Similarly, ilio-femoral bypass was patent. However, significant narrowing of external iliac artery was reported in two patients (one from group B and one from group C) 12 months post balloon angioplasty. These patients were primarily deemed not suitable for stenting. Recurrent stenoses were successfully dilated and stents were implanted.
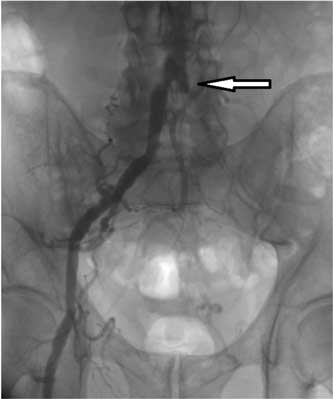
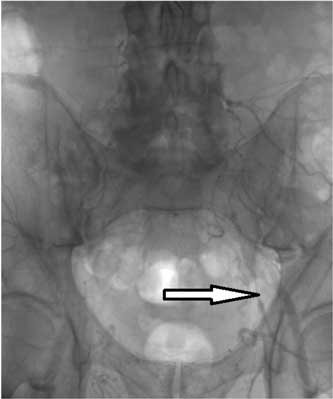
Fig. 1. 75 ys old male, claudication 50 m. Angiogram depicts left common iliac artery (LCIA) occlusion. (Arrow depicts LCIA stump.).
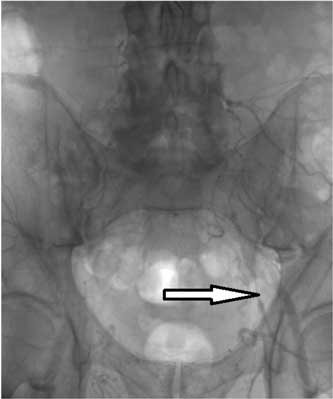
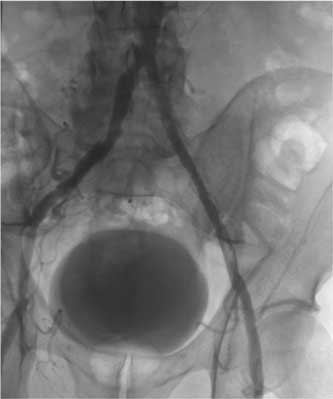
Fig. 2. Late chase of angiogram reveals delayed filling of left external iliac artery (arrow).
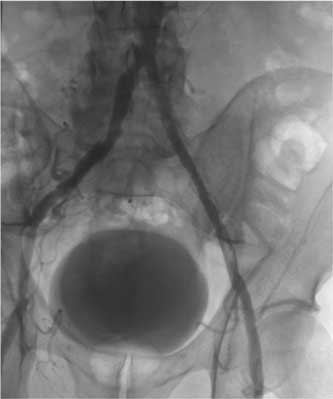
Fig. 3. Satisfactory flow through recanalised and angioplasted segment of left common iliac artery.
DISCUSSION
Iliac arteries occlusion is considered to be a challenge in endovascular surgery (4-6). The results obtained in our clinic are encouraging and the treatment is highly recommended in patients with significant comorbidities, when there is high risk of classic operation. Although endovascular treatment is regarded to be less invasive, we should remember of potential complications. Iliac artery perforation at the site of angioplasty is a serious one. Lack of complication usually causes an operator to minimize his vigilance. Consequently one can fail to notice vessel rupture. High pressure balloon angioplasty can cause abdominal pain, which soon subsides. However, if the pain persist, and patient becomes hypotensive, one should anticipate artery rupture unless proven otherwise (6-8). This complication should be recognized during primary operation. Delayed diagnosis in such case can lead to shock and death. If a rupture is extensive, finding a place of leakage is usually not difficult. Displacement of the urinary bladder laterally to the ruptured artery is an indirect symptom of arterial iatrogenic injury (9). In our study, such arterial injury was hopefully diagnosed upon angiogram already during the operation. Endovascular technique provides opportunity to seal a perforated vessel using a balloon, stent or even a stentgraft (7, 10, 11). In above mentioned case of iatrogenic iliac artery rupture, patient has been scheduled for open surgery following failed attempt to control bleeding by endovascular method (two stents implanted).
False aneurysm following femoral artery puncture is another potential complication of endovascular access. Arterial puncture site becomes a source of bleeding. Blood outflow creates a reservoir in the surrounding tissues. The reservoir communicates with a damaged artery through a channel called the neck. Obliterating of an aneurysm by prolonged compression with an ultrasound probe or an injection of thrombin into its lumen are therapeutic methods of choice (12-14). In our clinic, we used an effective thrombin injection performed under ultrasound control.
Distal emboli are a relatively common (10%) complication of iliac artery angioplasty. In patients presenting with intermittent claudication, distal emboli can increase ischaemic symptoms and cause early amputation (15, 16). In our material, 2 patients (4.3%) were diagnosed with distal emboli. Patient with blue toe syndrome was successfully treated conservatively, while the other was treated by local catheter directed thrombolysis. Both avoided ablation.
In summary we need to note, that complications following percutaneous iliac artery angioplasty are relatively rare and benign. Alternative ilio-femoral bypass graft surgery is linked with significantly higher morbidity. Therefore, iliac artery angioplasty should be recommended as a first choice therapy for atherosclerosis of this segment.
Many authors describe long-term results of iliac artery angioplasty as more and more satisfactory. Patency a year following PTA is within range of 90-97%, whilst four years patency is within 76-78% (15-17). In our material, midterm results were also very favourable. Two patients required successful angioplasty for stenosis, which gives a satisfactory result of 100% primary assisted patency one year following primary intervention. Long-term patency of the iliac arteries is still being investigated.
CONCLUSIONS
1. All TASC types of chronic iliac artery occlusion can be successfully managed using intravascular methods, with acceptable complication and conversion to open surgery rate.
2. Midterm results (annual primary assisted patency) have been very satisfactory.
3. Long-term patency of iliac artery angioplasty still require further investigation.
Piśmiennictwo
1. Norgren L, Hiatt WR, Dormandy JA et al.: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 2007; 33 Suppl 1: 1-75. 2. Galaria II, Davies MG: Percutaneous transluminal revascularization for iliac occlusive disease: Long term outcomes in TASC A and B lesions. Ann Vasc Surg 2005; 19: 352-360. 3. Leville CD, Kashyap VS, Clair DG et al.: Endovascular management of iliac artery occlusions: extending treatment to TASC C and D patients. J Vasc Surg 2006; 43:32-39. 4. Grodowski M, Motyka M, Ruciński T, Boczej R: Endovascular treatment of Leriche’s syndrome – a case report. Acta Angiol 2010; 16: 78-84. 5. Krankenberg H, Schlüter M, Schwencke C et al.: Endovascular reconstruction of the aortic bifurcation in patients with Leriche syndrome. Clin Res Cardiol 2009; 98: 657-664. 6. Pernès JM, Auguste MA, Hovasse D et al.: Long iliac stenosis: initial clinical experience with the Cragg endoluminal graft. Radiology 1995; 196: 67-71. 7. Chatziioannou A, Mourikis D, Katsimilis J et al.: Acute iliac artery rupture: endovascular treatment. Cardiovasc Intervent Radiol 2007; 30: 281-285. 8. Hamilos MI, Kochiadakis GE, Hatzidakis AA et al.: Treatment of a large rupture of the external iliac artery by implantation of a coated metal stent. Hellenic J Cardiol 2005; 46: 354-355. 9. Lois JF, Takiff H, Schechter MS et al.: Vessel rupture by balloon catheters complicating chronic steroid therapy. Am J Roentgenol 1985; 144: 1073-1074. 10. Sobrinho G, Albino JP: Delayed rupture of the external iliac artery after balloon angioplasty and stent placement. J Vasc Interv Radiol 2008; 19: 460-462. 11. Trehan V, Nigam A, Ramakrishnan S: Iatrogenic iliac artery rupture: emergency management by longer stent-graft on a shorter balloon. Cardiovasc Intervent Radiol 2007; 30: 108-110. 12. Kang SS, Labropoulos N, Mansour MA, Baker WH: Percutaneous ultrasound guided thrombin injection: a new method for treating postcatheterization femoral pseudoaneurysms. J Vasc Surg 1998; 27: 1032-1038. 13. Calton WC, Franklin DP, Elmore JR, Han DC: Ultrasound-guided thrombin injection is a safe and durable treatment for femoral pseudoaneurysms. Vasc Surg 2001; 35: 379-383. 14. Krueger K, Zaehringer M, Strohe D et al.: Postcatheterization pseudoaneurysm: results of US-guided percutaneous thrombin injection in 240 patients. Radiology 2005; 236: 1104-1110. 15. Vorwerk D, Guenther RW, Schürmann K et al.: Primary stent placement for chronic iliac artery occlusions: follow-up results in 103 patients. Radiology 1995; 194: 745-749. 16. Scheinert D, Schröder M, Ludwig J, Bräunlich S, Möckel M, Flachskampf FA, Balzer JO, Biamino G: Stent-supported recanalization of chronic iliac artery occlusions. Am J Med 2001; 110: 708-715. 17. Uher P, Nyman U, Lindh M et al.: Long-term results of stenting for chronic iliac artery occlusion. J Endovasc Ther 2002; 9: 67-75.