© Borgis - Postępy Nauk Medycznych 12/2014, s. 823-827
*Lucyna Papierska, Karolina M. Nowak
Obustronne guzy nadnerczy z podkliniczną hiperkortyzolemią. Operować czy obserwować?
Bilateral adrenal tumors with subclinical hypercortisolemia. To operate or observe?
Department of Endocrinology, Centre of Postgraduate Medical Education, Warszawa
Head of Department: prof. Wojciech Zgliczyński, MD, PhD
Streszczenie
Subkliniczna hiperkortyzolemia powodowana przez łagodne guzy nadnerczy według wielu źródeł stanowi automatyczne wskazanie do adrenalektomii. Jednakże niektóre prace oceniające wyniki leczenia operacyjnego zwracają uwagę na brak u wielu chorych jakiejkolwiek korzyści klinicznej z przebytego zabiegu. Również obserwowaliśmy to zjawisko w dużej serii chorych leczonych w naszej klinice.
Prezentujemy trzy przypadki kobiet pochodzące z obserwowanej przez nas grupy z obustronnymi łagodnymi guzami nadnerczy przebiegającymi z podkliniczną hiperkortyzolemią. Mimo podobnych wyników badań hormonalnych przebieg choroby był inny w każdym z opisanych przypadków. Jedynie u jednej z dwóch operowanych kobiet ustąpienie hiperkortyzolemii doprowadziło do poprawy stanu klinicznego. U nieoperowanej chorej nie obserwowano rozwoju jawnego klinicznie zespołu Cushinga. Nadciśnienie tętnicze, cukrzyca i otyłość nie muszą wynikać z hiperkortyzolemii i stąd ustąpienie zaburzeń hormonalnych po skutecznej adrenalektomii nie powoduje poprawy klinicznej u każdego pacjenta. Decyzja o leczeniu operacyjnym nie może opierać się jedynie na wynikach badań hormonalnych.
Summary
According to various sources, subclinical hypercortisolemia caused by benign adrenal tumors shows unquestionable indication to adrenalectomy. However, some works assessing effects of such surgery revealed no clinical benefits due to operation in some patients. We have also noted this fact in big series of patients treated in our clinic.
We present three cases of women from the group observed by us with bilateral benign adrenal tumors with subclinical hypercortisolemia. Despite similar results of hormonal examinations, the course of disease was different in the described cases. Only in one of two operated women regression of hypercortisolemia led to clinical improvement. In the non-operated one the development of overt Cushing syndrome has not been observed. Hypertension, diabetes and obesity not always are caused by hypercortisolemia – thus regression of hormonal disturbances after a successful adrenalectomy doesn‘t lead to a clinical improvement in all the patients. The approval of patients for surgery must not be based only on results of hormonal testing.

Introduction
The problem of incidentally detected bilateral adrenal tumors (incidentaloma) can be examined in several different ways. First of all, if such lesions are found, an „oncological vigilance” is obligatory as they might be bilateral neoplastic metastases (1). A quick differential diagnosis of metastatic lesions is possible by means of CT examinations during which the so-called imaging phenotype of tumors is assessed. Malignant lesions are characterized by a high coefficient of X-ray attenuation (density) prior to the administration of contrast medium and a low absolute and relative coefficients of contrast washout (which indicates a slow washout of the contrast medium in practice). Lipids are not found in such lesions on MRI (the assessment consists in comparing in-phase and antiphase signals produced by the tumor) (2, 3). A lack of lipids in the tumors might also give rise to suspicion of bilateral phaeochromocytomas – the presence of such lesions can be expected in patients with multiple endocrine neoplasia syndrome, whereas they are almost never present in other patients (4). Thus, it can be summarized that a detection of tumors containing no lipids in both adrenal glands is a definite indication for surgery after carrying out extended diagnostics (imaging examinations for detection of primary lesion in case of metastasis, a determination of 24-hour urinary catecholamines/metoxycatecholamines excretion, a MIBG scintigraphy and examinations for detection of other endocrinopathies in case of suspected phaeochromocytomas).
In case of bilateral adrenal incidentalomas, an assessment of their hormonal function is the second direction of actions. An excessive production of all the three groups of adrenocortical hormones (glucocorticoids, mineralocorticoids, androgens) and its autonomization may occur. In case of unilateral adrenal adenomas that show a subclinical hormonal function, the decision to perform surgery is usually taken. Adenomas can also occur as bilateral tumors with benign imaging phenotype, but they develop more often in the course of ACTH-independent macronodular adrenal hyperplasia (AIMAH) than in the case of unilateral lesions. A suspicion of hyperplasia changes the management method in case of detection of autonomous aldosterone production: a unilateral adenoma that causes a Conn’s syndrome is an indication for surgery, but a bilateral hyperplasia should be treated pharmacologically (5, 6). In case of hyperandrogenism with bilateral adrenal enlargement (with or without tumors) one may suspect an undiagnosed so far unclassical form of congenital adrenal cortical hyperplasia or hyperplasia of the reticular zone, which are also not an indication for operative treatment. Subclinical hypercortisolemia was for many years a definite indication for adrenalectomy (7, 8). However, recently arguments for a more cautious approach when making decisions on this operation were provided as it, even with an evident autonomization and increased cortisol secretion, does not always bring about a clinical improvement (9-11). The cases below from a large group of patients with bilateral adrenal tumors treated and observed in our teaching hospital department are illustrative of this problem.
Case 1
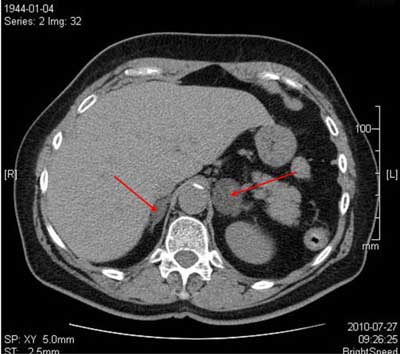
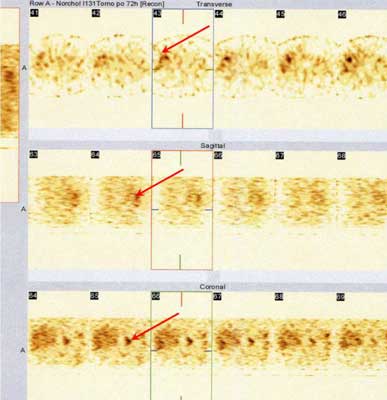
A 66-year-old woman with overweight (BMI 29 kg/m2), hyperinsulinism diagnosed during OGTT, poorly controlled arterial hypertension (> 140/90 mmHg, 5 antihypertensive drugs) and hyperlipidemia has been admitted to the Teaching Hospital Department of Endocrinology of the Centre of Postgraduate Medical Education because of bilateral adrenal tumors detected during an abdominal cavity ultrasonography. An imaging assessment was carried out and the following lesions were visualized on abdominal CT: a lesion 32 x 30 mm in size in the left adrenal gland and a lesion 21 x 11 mm in size in the right adrenal gland that had a density of +4 Hounsfield units (HU) and from -1 to +1 HU, respectively (fig. 1). A normal renin/aldosteron ratio (RAA), a normal concentration of adrenal androgens, normal both cortisol concentrations and circadian rhythm of cortisol excretion with a low morning ACTH concentration of 5 pg/ml were found in the hormonal evaluation. A lack of cortisol suppression (4.8 μg/dl) was found in the test performed with a dexamethasone (1 mg dose). In order to confirm the diagnosis of secretion autonomization and identify the secreting side, a radio-labelled norcholesterol (NP-59) scintigraphy of the adrenal glands was carried out and a predominant radiotracer uptake in the left adrenal gland was found (fig. 2). In consideration of the diagnosed autonomous hormonal function, the female patient has been approved for a laparoscopic removal of the left adrenal gland. A macronodular adrenocortical hyperplasia was found during a histopathological examination of the tumor. After the operative procedure, the female patient required substitutive doses of hydrocortisone for half a year due to the insufficiency of the other adrenal gland (during the 2nd month after surgery, the morning concentration of cortisol was 6.1 μg/dl, ACTH 2 pg/ml and 17-OHCS 2.1 mg in 24-hour urine collection), which definitely confirmed the preoperative diagnosis of subclinical hypercortisolemia. During the first six months after surgery, a decrease in body mass occured (down to BMI 23 kg/m2), the control of arterial pressure improved, which enabled a reduction of the doses of hypotensive drugs (at present, she is treated with sartan and a calcium channel blocker). The concentration of triglycerides, cholesterol-LDL fraction decreased.
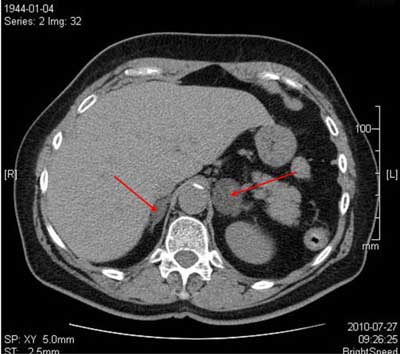
Fig. 1. Abdominal CT in patient No 1: bilateral lesions L > P.
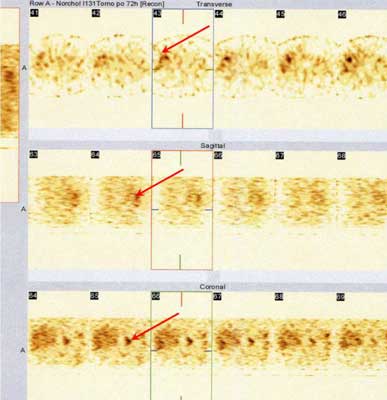
Fig. 2. NP-59 scintigraphy in patient No 1: predominant uptake in left adrenal gland.
Case 2
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
29 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
69 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
129 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 78 zł
Piśmiennictwo
1. Young WF Jr: The Incidentally Discovered Adrenal Mass. N Engl J Med 2007; 356: 601-610.
2. Ilias I, Sahdev A, Reznek R et al.: The optimal imaging of adrenal tumors: a comparison of different methods. Endocrine-Related Cancer 2007; 14: 587-599.
3. Podgórska J, Cieszanowski A, Bednarczuk T: Adrenal imaging. Pol J Endocrinol 2012; 63(1): 71-81.
4. Blake MA, Kalra MK, Maher MM et al.: Pheochromocytoma: An Imaging Chameleon. Radio Graphics 2004; 24: 87-99.
5. Hyla-Klekot L, Kokot F: Primary aldosteronism: a new insight into pathogenesis, diagnosis, and treatment in hypertensive patients. Pol Arch Med Wewn 2013; 123(10): 547-551.
6. Myśliwiec J, Górska M: Primary aldosteronism: a common and important problem. A practical guide to the diagnosis and treatment. Endokrynol Pol 2012; 63(4): 324-336.
7. Toniato A, Merante-Boschin I, Opocher G et al.: Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Annals of Surgery 2009; 249: 388-391.
8. Chiodini I, Morelli V, Salcuni AS et al.: Beneficial metabolic effects of prompt surgical treatment in patients with an adrenal incidentaloma causing biochemical hypercortisolism. J Clin Endocrinol Metab 2010; 95(6): 2736-2745.
9. Sereg M, Szappanos A, Toke J et al.: Atherosclerotic risk factors and complications in patients with non-functioning adrenal adenomas treated with or without adrenalectomy: a long-term follow-up study. Eur J Endocrinol 2009; 160: 647-655.
10. Papierska L, Ćwikła J, Rabijewski M et al.: Bilateral adrenal incidentaloma with subclinical hypercortisolemia: indications for surgery. Pol Arch Med Wewn 2014; 124(7-8): 387-394.
11. Terzolo M, Pia A, Reimondo G: Subclinical Cushing’s syndrome: definition and management. Clin Endocrinol (Oxf) 2012 Jan; 76(1): 12-18.
12. Terzolo M, Pia A, Ali A: Adrenal incidentaloma: a new cause of the metabolic syndrome? Journal of Clinical Endocrinology and Metabolism 2002; 87: 998-1003.
13. Rossi R, Tauchmanova L, Luciano A et al.: Subclinical Cushing’s syndrome in patients with adrenal incidentaloma: clinical and biochemical features. J Clin Endocrinol Metab 2000; 85: 1440-1448.
14. Terzolo M, Bovio S, Pia A et al.: Midnight serum cortisol as a marker of increased cardiovascular risk in patients with a clinically inapparent adrenal adenoma. Eur J Endocrinol 2005; 153: 307-315.
15. Vassilatou E, Vryonidou A, Michalopoulou S et al.: Hormonal activity of adrenal incidentalomas: results from a long-term follow-up study. Clinical Endocrinology 2009; 70: 674-679.
16. Giordano R, Marinazzo E, Berardelli R et al.: Long-term morphological, hormonal, and clinical follow-up in a single unit on 118 patients with adrenal incidentalomas. European Journal of Endocrinology 2010; 162: 779-785.
17. Erbil Y, Ozbey N, Barbaros U et al.: Cardiovascular risk in patients with nonfunctional adrenal incidentaloma: myth or reality? World Journal of Surgery 2009; 33: 2099-2105.
18. Papierska L: Taktyka postępowania diagnostycznego i terapeutycznego w przypadku obustronnych incydentaloma nadnerczy przebiegających z podkliniczną hiperkortyzolemią. Postępy Nauk Medycznych 2013; 3: 1-46.
19. Elahi-Moghaddam Z, Behnam-Rassouli M, Mahdavi-Shahri N et al.: Comparative study on the effects of type 1 and type 2 diabetes on structural changes and hormonal output of the adrenal cortex in male Wistar rats. Journal of Diabetes & Metabolic Disorders 2013; 12(9): 1-6.
20. Reincke M, Fassnacht M, Väth S et al.: Adrenal incidentalomas: a manifestation of the metabolic syndrome? Endocr Res 1996 Nov; 22(4): 757-761.
21. Miyazato M, Ishidoya S, Satoh F et al.: Surgical outcomes of laparoscopic adrenalectomy for patients with Cushing’s and subclinical Cushing’s syndrome: a single center experience. Int Urol Nephrol 2011; 43: 975-981.
22. Iacobone M, Albiger N, Scaroni C et al.: The Role of Unilateral Adrenalectomy in ACTH Independent Macronodular Adrenal Hyperplasia (AIMAH). World J Surg 2008; 32: 882-889.
23. Midorikawa S, Sanada H, Hashimoto S et al.: The improvement of insulin resistance in patients with adrenal incidentaloma by surgical resection. Clinical Endocrinology (Oxford) 2001; 54(6): 797-804.