Interdisciplinary (surgical and orthodontic) treatment in a patient with compound odontoma associated with impacted permanent lateral incisor of the mandible – a case report
Leczenie interdyscyplinarne (chirurgiczno-ortodontyczne) zębiaka zestawnego związanego z zatrzymanym stałym siekaczem bocznym żuchwy – opis przypadku
Impacted teeth are one of the reasons for orthodontic appointments. Two conditions must be met for the tooth to be considered impacted, i.e. a fully developed tooth that has not erupted on time. A fully impacted tooth is completely embedded in the bone, whereas a partially impacted tooth is covered with mucosa or only a fragment of the tooth’s crown is erupted (1). There are a number of reasons for the presence of impacted teeth, such as e.g. lack of space in the dental arch (due to a tendency to reduce mandibular and maxillary bones in the course of evolution as well as inconsistencies in the number and size of teeth), traumatic and genetic factors, inflammatory processes within the bone, vitamin A and D deficiency, and endocrine disorders. Impacted teeth also occur in syndromes, e.g. cleidocranial dysostosis (1, 2). The presence of odontoma in the maxillary bone when impacted teeth are observed is a particular situation. We present a case of a compound odontoma located in the anterior part of the mandible and associated with impacted permanent right lateral incisor of the mandible.
The aim of the study was to present the advances in interdisciplinary (surgical and orthodontic) treatment of a compound odontoma associated with the impacted permanent right lateral incisor of the mandible and a review of relevant literature.
A literature review covering years 1990-2016 was performed. Medical databases, such as PubMed and Medline, were used. The following keywords were used: “impacted”, “odontoma”, “orthodontic treatment”. Additionally, a manual search of specialist literature regarding orthodontics and maxillofacial surgery was conducted. Polish and English-language publications were included.
A 17-year-old female patient reported to the Orthodontic Clinic in the Specialist Hospital in Radom for consultation and treatment due to a persistent mandibular right lateral incisor and a bulging on the internal surface of the mandible. No significant family or general medical history was reported. No previous trauma or infections in the anterior mandible were reported. Extraoral examination revealed no abnormalities. Intraoral examination revealed mixed dentition, and in the right mandible: a persistent primary lateral incisor, the lack of permanent lateral incisor and oedema of the inner surface of the anterior mandible (fig. 1a-e). The adjacent teeth (mandibular canine tooth and mandibular canine tooth on the right side) showed normal colour and reaction to ethyl chloride. The surrounding mucous membrane was smooth, pink, moist and shiny. Orthodontic examination showed Angle’s Class II tendency and 1/2 of cuspid class II on the right, Angle’s Class I and cuspid class I on the left, as well as: a midline shift of 3 mm to the right, minor maxillary and mandibular dental crowding.
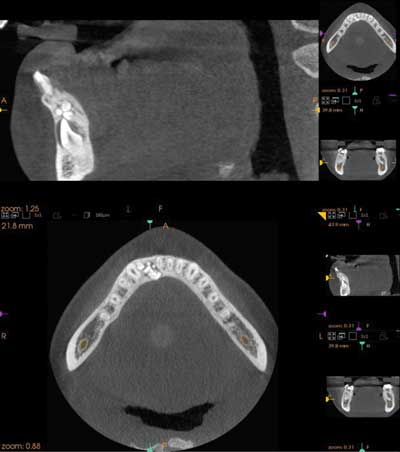
Panoramic radiography (fig. 2) showed an oval structure with clear borders and filled with a mass of small structures, probably corresponding to a compound odontoma. Cephalometry showed skeletal class I and anteriorotation (fig. 3). Cone beam computed tomography (CBCT) of the mandible was also preformed to precisely locate the lesion and plan treatment. CBCT showed no resorption of the teeth adjacent to the tumour, i.e. the medial incisor and the canine tooth (fig. 4).
After clinical and radiological examination, a preliminary diagnosis was made: a compound odontoma in the anterior part of the mandible, impacted mandibular right lateral incisor. The treatment plan included interdisciplinary, i.e. surgical and orthodontic, treatment. A two-stage surgical treatment was planned. In the first stage, surgical enucleation of the tumour was performed, while the second stage involved tooth exposure and positioning of a bracket on the tooth in order to apply orthodontic force. The aim of orthodontic treatment was to restore the site for the impacted permanent mandibular lateral incisor, and then introduce the tooth into the dental arch using orthodontic force. Written consent from the subject/subject’s parents/subject’s legal guardians was obtained.
1. Kryst L (red.): Chirurgia szczękowo-twarzowa. Wyd. V. Wydawnictwo Lekarskie PZWL, Warszawa 2007.
2. Szpringer-Nodzak M, Wochna-Sobańska M (red.): Stomatologia wieku rozwojowego. Wyd. IV. Wydawnictwo Lekarskie PZWL, Warszawa 2006.
3. Ferrer Ramírez MJ, Silvestre Donat FJ, Estelles Ferriol E et al.: Recurrent infection of a complex odontoma following eruption in the mouth. Med Oral 2001; 6(4): 269-275.
4. Kämmerer PW, Schneider D, Schiegnitz E et al.: Clinical parameter of odontoma with special emphasis on treatment of impacted teeth-a retrospective multicentre study and literature review. Clin Oral Investig 2016; 20(7): 1827-1835.
5. Thompson L: World Health Organization classification of tumours: pathology and genetics of head and neck tumours. Ear Nose Throat J 2006; 85(2): 74.
6. Reichart PA, Philipsen HP, Sciubba JJ: The new classification of head and neck tumours (WHO) – any changes? Oral Oncol 2006; 42(8): 757-758.
7. Barnes L, Everson J, Reichart P, Sidransky D: Pathology and Genetics of Head and Neck Tumors. IARC Press 2005; 285: 310-311.
8. Kruś S: Patomorfologia dla stomatologów. Wyd. I. Wydawnictwo Medyczne Med Tour Press International, Warszawa 1997.
9. Amado Cuesta S, Gargallo Albiol J, Berini Aytès L, Gay Escoda C: Review of 61 cases of odontoma. Presentation of an erupted complex odontoma. Med Oral 2003; 8(5): 366-373.
10. Katz RW: An analysis of compound and complex odontomas. ASDC J Dent Child 1989; 56(6): 445-449.
11. Tyangi P, Singla S: Complex composite odontoma. J Clin Pediatr Dent 2010; 3(2): 117-120.
12. Amailuk P, Grubor D: Erupted odontoma: case report of 15-year-old Sudanese boy with a history of traditional dental mutilation. Br Dent J 2008; 204: 11-14.
13. Serra-Serra G, Berini-Aytès L, Gay-Escoda C: Erupted odontomas: a report of three cases and review of the literature. Med Oral Patol Oral Cir Bucal 2009; 14(6): E299-E303.
14. Ragalli CC, Ferreria JL, Blasco F: Large erupting complex odontoma. Int J Oral Maxillofac Surg 2000; 29(5): 373-374.
15. Ajike SO, Adekeye EO: Multiple odontomas in the facial bones. A case report. Int J Oral Maxillofac Surg 2000; 29(6): 443-444.
16. Bereket C, Çakır-Özkan N, Şener I et al.: Complex and compound odontomas: Analysis of 69 cases and a rare case of erupted compound odontoma. Niger J Clin Pract 2015; 18(6): 726-730.
17. Kaczmarzyk T, Stypułkowska J, Tomaszewska R, Czopek J: Nowotwory zębopochodne i guzy nowotworopodobne kości szczękowych. Wyd. I. Wydawnictwo Kwintesencja, Warszawa 2009.
18. Tuczyńska A, Bartosik D, Abu-Fillat Y et al.: Compound odontoma in the mandible-case study and literature review. Dev Period Med 2015; 19(4): 484-489.
19. Stypułkowska J: Nowotwory zębopochodne i zmiany nowotworopodobne kości szczękowych. Studium kliniczne i ocena wyników leczenia. Folia Med Crac 1998; 39: 35-141.
20. Soluk Tekkesin M, Pehlivan S, Olgac V et al.: Clinical and histopathological investigation of odontomas: Review of the literature and presentation of 160 cases. J Oral Maxillofac Surg 2012; 70: 1358-1361.
21. Hidalgo Sánchez O, Leco Berroca ML, Martínez González JM: Metaanalysis of the epidemiology and clinical manifestations of odontomas. Med Oral Patol Oral Cir Bucal 2008; 13(11): E730-E734.
22. Buchner A, Merrell PW, Carpenter WM: Relative frequency of central odontogenic tumors: a study of 1088 cases from Northern California and comparison to studies from other parts of the Word. J Oral Maxillofac Sur 2006; 64(9): 1343-1352.
23. Mathew AK, Shenai P, Chatra I et al.: Compound odontoma in decidous dentition. Ann Med Health Sci Res 2013; 3(2): 285-287.
24. de Oliveira BH, Campos V, Marçal S: Compound odontoma-diagnosis and treatment: three case reports. Pediatr Dent 2001; 23(2): 151-157.
25. Murphy C, O’Connell JE, Cotter E, Kearns G: Management of large erupting complex odontoma in maxilla. Case Rep Pediatr 2014; 963962. DOI: 10.1155/2014/963962.
26. Abdul M, Pragati K, Yusuf C: Compound composite odontoma and its management. Case Rep Dent 2014; 107089. DOI: 10.1155/2014/107089.
27. Pippi R: Odontomas and supernumerary teeth: is there a common origin? Int J Med Sci 2014; 11(12): 1282-1297.
28. Khan N, Shrivastava N, Shrivasava TV, Samadi FM: An unusual case of compound odontoma associated with maxillary impacted central incisor. Natl J Maxillofac Surg 2014; 5(2): 192-194.
29. Raval N, Metha D, Vachhrajani K, Nimavat A: Erupted odontoma: a case report. JCDR 2014; 8(7): 10-11.
30. Garcia-Consuegra L, Junquera LM, Albertos JM, Rodriguez O: Odontomas. A clinical-histological and retrospective epidemiological study of 46 cases. Med Oral 2000; 5(5): 367-372.
31. Reichart PA, Philipsen HP: Odontogenic tumors and allied lesions. Quintessence Publishing, USA 2004.
32. Janas A, Grzesiak-Janas G: Zębiaki złożone. Dent Med Probl 2005; 42(3): 425-429.
33. Martín-Granizo-López R, López-García-Asenjo J, De-Pedro-Marina M, Domínguez-Cuadrado L: Odontoameloblastoma: a case report and a review of the literature. Med Oral 2004; 9(4): 340-344.
34. Iwamoto O, Harada H, Kusukawa J, Kameyama TJ: Multiple odontomas of the mandible: a case report. Oral Maxillofac Surg 1999; 57(3): 338-341.
35. An S, An C, Choi K: Odontoma: a retrospective study of 73 cases. Imaging Sci Dent 2012; 42: 77-81.
36. Kaban LB: Pediatric Oral and Maxillofacial Surgery. Saunders, Philadelphia 1995: 111-112.
37. Morning P: Impacted teeth in relation to odontomas. Int J Oral Surg 1980; 9(2): 81-91.
38. Ashkenazi M, Greenberg BP, Chodik G et al.: Postoperative prognosis of unerupted teeth after removal of supernumerary teeth or odontomas. Am J Orthod Dentofacial Orthop 2007; 131: 614-619.
39. Ledesma-Montes C, Perez-Bache A, Garcès-Ortíz M: Gingival compound odontoma. Int J Oral Maxillofac Surg 1996; 25(4): 296-297.
40. Tomizawa M, Otsuka Y, Noda T: Clinical observations of odontomas in Japanese children: 39 cases including one recurrent case. Int J Paediatr Dent 2005; 15(1): 37-43.
41. Kamakura S, Matsui K, Katou F et al.: Surgical and orthodontic management of compound odontoma without removal of the impacted permanent tooth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94(5): 540-542.
42. Nagaraj K, Upadhyay M, Yadav S: Impacted maxillary central incisor, canine, and second molar with 2 supernumerary teeth and an odontoma. Am J Orthod Dentofacial Orthop 2009; 135(3): 390-399.
43. Hisatomi MD, Asaumi JI, Konouchi H et al.: A case of complex odontoma associated with impacted lower deciduous second molar and analysis of the 107 odontomas. Oral Dis 2002; 8(2): 100-105.
44. Oliver RG, Hodhges CGL: Delayed eruption of maxillary central incisor associated with an odontome: report of case. ASCD J Dent Child 1988; 55: 368-371.
45. Iatrou I, Vardas E, Theologie-Lygidakis N, Leventis M: A retrospective analysis of the characteristics, treatment and follow-up of 26 odontomas in Greek children. J Oral Sci 2010; 52(3): 439-447.
46. Kokich VG, Mathews DP: Surgical and orthodontic management of impacted teeth. Dent Clin North Am 1993; 37(2): 181-204.
47. Mupparapu M, Singer SR, Rinaggio J: Complex odontoma of unusual size involving the maxillary sinus: report of a case and review of CT and histopathologic features. Quintessence Int 2004; 35(8): 641-645.
48. Kodali RM, Venkat Suresh B, Ramanjaneya Raju P, Vora SK: An Unusual Complex Odontoma. J Maxillofac Oral Surg 2010; 9(3): 314-317.