© Borgis - Postępy Nauk Medycznych 12/2015, s. 869-873
Agnieszka Łebek-Szatańska, *Waldemar Misiorowski, Wojciech Zgliczyński
Jatrogenna niedoczynność przytarczyc – nie tylko strumektomia...
Iatrogenic hypoparathyroidism – not only after thyroid surgery...
Department of Endocrinology, Centre of Postgraduate Medical Education, Bielański Hospital, Warszawa
Head of Department: prof. Wojciech Zgliczyński, MD, PhD
Streszczenie
Najczęstszą przyczynę niedoczynności przytarczyc stanowi leczenie operacyjne chorób tarczycy lub przytarczyc. Znacznie rzadziej niedoczynność przytarczyc jest wynikiem rozległych zabiegów chirurgicznych z przyczyn onkologicznych, np. z powodu raka krtani czy górnej części przełyku, lub radioterapii szyi, np. w przypadku chłoniaka. W tych szczególnych przypadkach onkologiczny charakter samej choroby skupia na sobie większość uwagi zarówno pacjentów, jak i lekarzy, co często prowadzi do zaniedbywania innych zagrożeń dla zdrowia, zaś potencjalnie złe rokowania i krótki czas przeżycia w tych przypadkach dodatkowo maskują problem. Jednak u poszczególnych pacjentów wyleczonych z raka, nierozpoznana niedoczynność przytarczyc może w dłuższej perspektywie wywierać istotny wpływ na zdrowie i jakość życia. Przedstawiamy dwa takie przypadki. Według naszej wiedzy, przedstawione przez nas przypadki są pierwszymi, rozpoznanymi po tak długim czasie po laryngektomii lub radioterapii. Może to oznaczać, że inni pacjenci poddani takiemu leczeniu mogą być podobnie narażeni na to rzadkie powikłanie, bez względu na okres czasu, który upłynął od terapii. Oznacza to konieczność systematycznego monitorowania kalcemii, jak również wykonywania rozszerzonej diagnostyki w przypadku najmniejszego podejrzenia klinicznego niedoczynności przytarczyc.
Summary
The most common causes of hypoparathyroidism are iatrogenic: mostly thyroid or parathyroid surgery. Much less frequently HypoPT is caused by an extensive oncological surgical procedure e.g. because of larynx or upper throat cancer, or external neck radiotherapy, e.g. in the case of lymphoma. In those particular cases, both patients and doctors focus their attention on the oncological nature of the disease itself, which often results in neglect of other health hazards, and potentially poor prognosis, and short survival time in those cases additionally mask the problem. However, in individual patients cured from cancer, unrecognized hypoparathyroidism can significantly affect their health and quality of life. Two such cases are presented. To our knowledge, the cases presented by us are the first cases diagnosed after such a long time after laryngectomy or radiation therapy. This may indicate that other patients undergoing such treatment could be exposed to this rare complication as well, regardless of the time that elapsed after the treatment. This implies the need for systematic monitoring of serum calcium, as well as for enhanced diagnosis in the case of even the slightest clinical suspicion of hypoparathyroidism.

Introduction
Hypoparathyroidism (HypoPT) is a disease of the endocrine system characterized by low serum calcium and inadequately low PTH level. It is a rare disease, entered on the list of orphan diseases by the European Commission in January 2014 (UE/3/13/1210; http://www.ema.europa.eu/ema/index.jsp?curlZpages/medicines/human/orphans/2014/01/human_orphan_001301.jsp&midZWC0b01ac058001d12b) and the only classical hormonal insufficiency, which is not treated by supplementing the missing hormone (PTH) (1-4). Spontaneous HypoPT may be a disease with autoimmune pathogenesis where the cause is a mutation of the autoimmune regulatory gene (AIRE) (5). In addition, there are many other rare genetic diseases that can cause HypoPT: either as part of a larger complex of diseases (e.g., DiGeorge syndrome), or as a single endocrinopathies (6). However, the most common causes of chronic HypoPT are of iatrogenic origin: surgical treatment of thyroid and parathyroid diseases (7, 8).
Much less frequently HypoPT is caused by an extensive oncological surgical procedure e.g. because of larynx or upper throat cancer, or external neck radiotherapy, e.g. in the case of lymphoma. In those particular cases, both patients and doctors focus their attention on the oncological nature of the disease itself, which often results in neglect of other health hazards, and potentially poor prognosis, and short survival time in those cases additionally mask the problem. However, in individual patients cured from cancer, unrecognized hypoparathyroidism can significantly affect their health and quality of life (9). Two such cases are presented.
Case 1
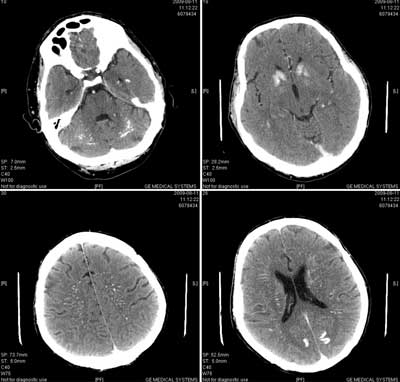
A 84-year-old male patient with a tracheotomy after surgical treatment of laryngeal cancer 30 years earlier, was admitted to the internal medicine ward diagnosed with pneumonia. Due to the very long period of time that has elapsed since the surgery, detailed information on the carried out procedure could not be obtained. The patient denied to have the history of radiotherapy. The immediate cause of hospitalization was a loss of consciousness for a few minutes while waiting for the medical appointment with the primary care physician. According to the statement of the patient, similar episodes have occurred many times in the past few years, but he did not report this problem to the doctor. The faints occurred mainly in stressful situations, and they were not connected with the changes in body position, without cardiovascular complaints, convulsions, involuntary urination, with no obvious prodromal symptoms. After combating the infection, the doctors started to diagnose the faints. Laboratory tests have shown the profound hypocalcemia: Ca = 1.31 mmol/l, ionized Ca = 0.73 mmol/l, and hypocalciuria Cau = 1.11 mmol/24 h; hyperphosphatemia p = 1.49 mmol/l, and an extremely low concentration of parathyroid hormone intact in the serum (iPTH) = 9.34 pg/ml. Diagnosis: secondary hypoparathyroidism following the laryngectomy. There were no classic signs of tetanic symptoms (Trousseau, Chvostek signs), however there were other clinical features of long hypocalcemia: prolongation of QT interval (QTc = 475 ms) in the electrocardiogram (ECG) and supraventricular and ventricular arrhythmias in 24-hour Holter ECG. A CT scan revealed the presence of massive calcification in the brain and cerebellum (as in Fahr’s disease) (fig. 1), but without clinical neurological disorders or pathologies in the electroencephalographic recordings. The examination showed cataract affecting both eyes. An attempt was made to perform a psychological evaluation, but due to significant difficulties in communication with the patient (hearing loss, speech disorders), as well as the advanced age, it was difficult to objectively assess his cognitive abilities. Treatment consisted in administration of calcium carbonate – 1000 mg three times a day, and alfacalcidol – 1 microgram per day. After two months of treatment a satisfactory improvement in the patient’s condition was achieved, fainting did not reappear, and the patient observed a significantly better efficiency of movement and improvement of mood. Laboratory studies confirmed improvement of serum calcium level (2.13 mmol/l) and normalization of phosphate level (1.11 mmol/l). ECG showed normalization of QT interval (QTc = 435 ms).
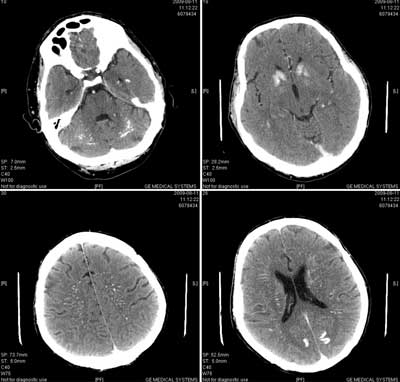
Fig. 1. Massive calcification of the brain with hypoparathyroidism.
Case 2
Powyżej zamieściliśmy fragment artykułu, do którego możesz uzyskać pełny dostęp.
Mam kod dostępu
- Aby uzyskać płatny dostęp do pełnej treści powyższego artykułu albo wszystkich artykułów (w zależności od wybranej opcji), należy wprowadzić kod.
- Wprowadzając kod, akceptują Państwo treść Regulaminu oraz potwierdzają zapoznanie się z nim.
- Aby kupić kod proszę skorzystać z jednej z poniższych opcji.
Opcja #1
29 zł
Wybieram
- dostęp do tego artykułu
- dostęp na 7 dni
uzyskany kod musi być wprowadzony na stronie artykułu, do którego został wykupiony
Opcja #2
69 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 30 dni
- najpopularniejsza opcja
Opcja #3
129 zł
Wybieram
- dostęp do tego i pozostałych ponad 7000 artykułów
- dostęp na 90 dni
- oszczędzasz 78 zł
Piśmiennictwo
1. Bollerslev J, Rejnmark L, Marcocci C et al.: European Society of Endocrinology Clinical Guideline: Treatment of chronic hypoparathyroidism in adults. European Journal of Endocrinology 2015; 173: G1-G20.
2. Bilezikian JP, Khan A, Potts JT Jr et al.: Hypoparathyroidism in the Adult: Epidemiology, Diagnosis, Pathophysiology, Target-Organ Involvement, Treatment, and Challenges for Future Research. J Bone Miner Res 2011; 26(10): 2317-2337.
3. Khan MI, Waguespack SG, Hu MI: Medical management of postsurgical hypoparathyroidism. Endocr Pract 2011; 17 (suppl. 1): 18-25.
4. Shoback D: Clinical practice. Hypoparathyroidism. N Engl J Med 2008; 359(4): 391-403.
5. Betterle C, Garelli S, Presotto F: Diagnosis and classification of autoimmune parathyroid disease. Autoimmun Rev 2014; 13(4-5): 417-422.
6. Lima K, Abrahamsen TG, Wolff AB et al.: Hypoparathyroidism and autoimmunity in the 22q11.2 deletion syndrome. Eur J Endocrinol 2011; 165(2): 345-352.
7. Bohrer T, Hagemeister M, Elert O: A clinical chameleon: postoperative hypoparathyroidism. Langenbecks Arch Surg 2007; 392(4): 423-426. Epub 2006 Nov 28.
8. Puzziello A, Rosato L, Innaro N et al.: Hypocalcemia following thyroid surgery: incidence and risk factors. A longitudinal multicenter study comprising 2,631 patients. Endocrine 2014 Nov; 47(2): 537-542.
9. Underbjerg L, Sikjaer T, Mosekilde L, Rejnmark L: Cardiovascular and renal complications to postsurgical hypoparathyroidism: a Danish nationwide controlled historic follow-up study. J Bone Miner Res 2013; 28(11): 2277-2285.
10. Sitges-Serra A, Ruiz S, Girvent M: Outcome of protracted hypoparathyroidism after parathyroidectomy. Br J Surg 2010; 97: 1687-1695.
11. Page C, Strunski V: Parathyroid risk in total thyroidectomy for bilateral, benign, multinodular goitre: report of 351 surgical cases. J Laryngol Otol 2007; 121: 237-241.
12. Thomusch O, Machens A, Sekulla C et al.: The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: a multivariate analysis of 5846 consecutive patients. Surgery 2003; 133: 180-195.
13. Welch KC, McHenry CR: Total thyroidectomy: is morbidity higher for Graves’ disease than nontoxic goiter? J Surg Res Epub ahead of print 19 April 2011.
14. Basheeth N, O’Cathain E, O’Leary G, Sheahan P: Hypocalcemia after total laryngectomy: incidence and risk factors. Laryngoscope 2014; 124(5): 1128-1133.
15. Lo Galbo AM, Kuik DJ, Lips P et al.: A prospective longitudinal study on endocrine dysfunction following treatment of laryngeal or hypopharyngeal carcinoma. Oral Oncology 2013; 49: 950-955.
16. Thorp MA, Levitt NS, Mortimore S, Isaacs S: Parathyroid and thyroid function five years after treatment of laryngeal and hypopharyngeal carcinoma. Clin Otolaryngol Allied Sci 1999; 24(2): 104-108.
17. Fajardo LF: Pathology of Radiation Injury. Masson Publishing, USA, New York 1982: 206-212.
18. Holden I, Christiansen C: Unchanged parathyroid gland function following irradiation for malignances of the head and neck. Cancer 1984; 33: 874-877.
19. Eipe J, Johnson SA, Kiamko RT et al.: Hypoparathyroidism following 131I therapy for hyperthyoidism. Arch Intern Med 1968; 121: 270-271.
20. Glazbrook GA: Effect of decicurie dose of radioactive iodine 131I on parathyroid function. Am J Surg 1987; 154: 368-373.
21. Cusano NE, Maalouf NM, Wang PY et al.: Normocalcemic Hyperparathyroidism and Hypoparathyroidism in Two Community-Based Nonreferral Populations. J Clin Endocrinol Metab 2013; 98(7): 2734-2741.
22. Arlt W, Fremerey C, Callies F et al.: Well-being, mood and calcium homeostasis in patients with hypoparathyroidism receiving standard treatment with calcium and vitamin D. Eur J Endocrinol 2002; 146(2): 215-222.
23. Underbjerg L, Sikjaer T, Mosekilde L, Rejnmark L: Postsurgical hypoparathyroidism – risk of fractures, psychiatric diseases, cancer, cataract, and infections. J Bone Miner Res 2014; 29: 2504-2510.
24. Illum F, Dupont E: Prevalences of CT-detected calcification in the basal ganglia in idiopathic hypoparathyroidism and pseudohypoparathyroidism. Neuroradiology 1985; 27: 32-37.
25. Faig JC, Kalinyak J, Marcus R et al.: Chronic atypical seizure disorder and cataracts due to delayed diagnosis of pseudohypoparathyroidism. West J Med 1992; 157: 64-65.
26. Basser LS, Neale FC, Ireland AW et al.: Epilepsy and electroencephalographic abnormalities in chronic surgical hypoparathyroidism. Ann Intern Med 1969; 71: 507-515.
27. Kelly R, Taggart H: Hypoparathyroidism – presenting 40 years after thyroid surgery. Ulster Med J 1998; 67(1): 63-64.