© Borgis - New Medicine 4/2010, s. 166-168
*Ewa Ogłodek, Aleksander Araszkiewicz
The Montgomery-Asberg Depression Rating Scale (MADRS) in diagnosis of depressive disorder in a female patient with psoriasis
Chair and Clinic of Psychiatry of the Nicolaus Copernicus University,
Collegium Medicum in Bydgoszcz, Poland
Head of Department: prof. Aleksander Araszkiewicz, MD, PhD
Summary
Psoriasis is one of the most common chronic inflammatory skin diseases, with a complex, multifactorial and still not fully understood aetiopathogenesis. It is estimated that approximately 1-2% of the general population of highly developed countries has psoriasis. Psoriasis is also associated with limitations in daily activities, occupational, and sexual functioning. Patients with psoriasis suffer comparable disability as other patients with mental illnesses. People with psoriasis have a greater risk of depression, anxiety, and suicidal thoughts. This chronic condition has a significant negative impact on patients? quality of life. Depression and a reduced quality of life significantly affect patients with psoriasis. The aim of the study was to evaluate the effectiveness of depression treatment in a patient with psoriasis.
Material and method. A 48-year-old female patient, suffering from a DSM-IV major depressive episode and psoriasis, was examined with the Montgomery-Asberg Depression Rating Scale (MADRS) before and after treatment with mirtazapine.
Results. Mean MADRS scores changed from 37 to 9.
Aim. The patient reached remission of depression after 12 weeks of pharmacological treatment with mirtazapine.
Conclusions. 1. There is a relation between psoriasis and falling ill with depression. 2. Mirtazapine proved to be an effective medication in the treatment of the patient with depression and psoriasis.
Introduction
Most dermatological disorders influenced by psychosocial factors are associated with both psychosocial stress, which exacerbates a person?s general condition, and psychological and psychiatric diseases, such as depression, anxiety disorders, and body image problems (1).
Psoriasis, a common skin complaint, affects an estimated 1-3% of the world population. Among several clinical phenotypes chronic plaque psoriasis is the most frequent and accounts for about 90% of cases. Psoriasis may cause substantial problems in everyday life.
Several studies suggest that patients with severe psoriasis have an increased risk for depressive illness, and a decreased life expectancy (2). Currently incurable, psoriasis causes remarkable direct costs, work limitations and productivity loss. When psoriasis starts worsening, patients are subjected to increased stress. They have often been noted to be obsessed with the progressing disease and suffer from dysthymia and depression (3). Depression and suicidal ideation have been noted in patients severely affected by psoriasis and their prevalence was found to be higher than in general medical patients (4).
Material and Method
A 48-year-old female patient, suffering from a DSM-IV major depressive episode and psoriasis, was examined twice with the Montgomery-Asberg Depression Rating Scale (MADRS): before treatment with the antidepressant, and 2 months after the therapy began.
The Montgomery-Asberg Depression Rating Scale (abbreviated MADRS) is a 10-item diagnostic questionnaire which psychiatrists use to measure the severity of depressive episodes in patients with mood disorders. The 10 items measure several dimensions of depressive symptomatology such as apparent and reported sadness, inner tension, reduced sleep, reduced appetite, loss of concentration, lassitude, inability to feel, pessimistic thoughts and suicidal ideas. The MADRS divides the severity into grades 0 to 6 (5). The patient was treated with mirtazapine. Mirtazapine was given over 12 weeks in a dose of 45 mg/day at bedtime. Therapeutic response was defined as a 50% decrease on the MADRS.
Results
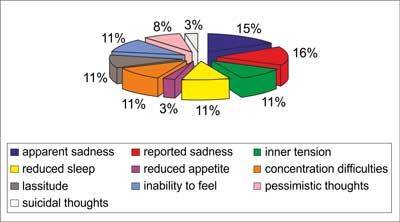
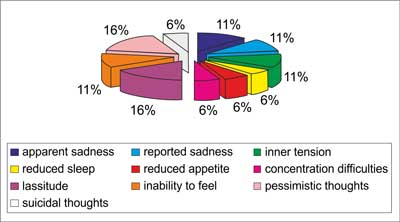
The diagnosis of depression was made according to the DSM-IV criteria for major depressive episode. Patients were further characterized with the DSM-IV specifiers for melancholy, atypical depression, severity of depression (mild, moderate, severe with psychotic symptoms, severe without psychotic symptoms), and recurrence. Mean MADRS scores changed from 37 to 9. Figures 1 and 2 present the percentage distribution of the 10 items of MADRS before treatment with mirtazapine and 12 weeks after the treatment began. The patient reached remission of depression after 12 weeks of treatment with mirtazapine.
Fig. 1. The Montgomery-Asberg Depression Scale before pharmacological therapy with mirtazapine.
Fig. 2. The Montgomery-Asberg Depression Scale after 12 weeks of pharmacological therapy with mirtazapine.
Discussion
Psoriasis is a common chronic, inflammatory, proliferative and papulosquamous disease of the skin. When psoriasis starts worsening, patients are subjected to increased stress. They have often been noted to be obsessed with the progressing disease and suffer from dysthymia and depression (6).
In the study conducted by Bilac C. et al., all the patients had more than 30% body surface area involved and the disease was progressing rapidly. All were suffering from severe stress due to the progress of the disease (7).
In the female patient described, mirtazapine was applied and brought positive therapeutic results. Mirtazapine enhances noradrenaline and serotonin neurotransmission by its direct effect on various alpha-adrenergic and serotonergic receptors. Mirtazapine increases the release of noradrenaline by blocking the alpha-2 presynaptic adrenoceptors (8). The increase of intrasynaptic noradrenaline concentration activates in turn the alpha-1 adrenoceptors located on serotonergic neurons. Mirtazapine also has high antagonist affinity for the 5-HT2, 5-HT3, and H1 receptors (9). This prevents the overexcitation of serotonergic neurons and adds a sedative component to the spectrum of pharmacological actions of the drug. At the hormonal level, mirtazapine, unlike other antidepressants, reduces the release of corticotrophin and cortisol (10, 11).
Many reports suggest that stress affects the skin via the HPA axis. The skin is connected to the brain via the nervous system. Immunohistochemical and electron microscopic analyses have demonstrated the intimate association of epidermal Langerhans cells and a nerve fibre. The function of Langerhans cells was suppressed by the neuropeptide calcitonin gene-related peptide. Another neuropeptide, substance P, is increased after administration of immobilization stress. Hirschfeld R.M. et al. hypothesized that substance P is a regulator of stress reactions affecting the hair cycle. Catecholamines were reported to regulate the Langerhans cell functions (12).
Conclusions:
1. There is a relation between psoriasis and falling ill with depression.
2. Mirtazapine proved to be an effective medication in the treatment of the patient with depression and psoriasis.
Piśmiennictwo
1. De Bolle M, Johnson JG, De Fruyt F: Patient and clinician perceptions of therapeutic alliance as predictors of improvement in depression. Psychother Psychosom 2010; 79(6): 378-3. 2. Ogłodek E, Moś D, Araszkiewicz A: Coexisting of borreliosis, depression and psoriasis
? case report. Pol Merkur Lekarski 2010; 28(163): 53-5. 3. Esposito M et al.: An Italian study on psoriasis and depression. Dermatology 2006; 212(2): 123-7. 4. Langley RG et al.: Ustekinumab significantly improves symptoms of anxiety, depression, and skin-related quality of life in patients with moderate-to-severe psoriasis: Results from a randomized, double-blind, placebo-controlled phase III trial. J Am Acad Dermatol 2010; 63(3): 457-65. 5. Montgomery S, Hansen T, Kasper S: Efficacy of escitalopram compared to citalopram: a meta-analysis. Int J Neuropsychopharmacol 2010; 29: 1-8. 6. Menter A et al.: The effect of adalimumab on reducing depression symptoms in patients with moderate to severe psoriasis: a randomized clinical trial. J Am Acad Dermatol 2010; 62(5): 812-8. 7. Bilac C et al.: The relationship between symptoms and patient characteristics among psoriasis patients. Indian J Dermatol Venereol Leprol 2009; 75(5): 551. 8. Blier P et al.: Mirtazapine and paroxetine in major depression: a comparison of monotherapy versus their combination from treatment initiation. Eur Neuropsychopharmacol 2009; 19(7): 457-65. 9. Lavergne F et al.: Onset of improvement and response to mirtazapine in depression: a multicenter naturalistic study of 4771 patients. Neuropsychiatr Dis Treat 2005; 1(1): 59-68. 10. Mössner R et al.: Analysis of a functional serotonin transporter promoter polymorphism in psoriasis vulgaris. Arch Dermatol Res 2009; 301(6): 443-7. 11. Guelfi JD et al.: Mirtazapine versus venlafaxine in hospitalized severely depressed patients with melancholic features. J Clin Psychopharmacol 2001; 21(4): 425-31. 12. Hirschfeld RM et al.: Partial response and nonresponse to antidepressant therapy: current approaches and treatment options. J Clin Psychiatry 2002; 63(9): 826-37.