© Borgis - New Medicine 4/2010, s. 111-114
Mieczysław Chmielik, Jolanta Jadczyszyn, *Magdalena Frąckiewicz
Clinical results of plastic surgery of deviated nasal septum in developmental age
Department of Paediatric Otorhinolaryngology, Medical University of Warsaw, Poland
Head of Department: prof. Mieczysław Chmielik, MD, PhD
Summary
Introduction. Child nasal septum operation is a method implemented in clinical practice in the 1950s. Its performance in
Poland started in 1979. To date, over 3000 such operations have been performed and analysed in the Paediatric Otorhinolaryngology Clinic of the Medical University of Warsaw.
Aim. To perform an analysis of patients operated on because of deviation of the nasal septum during 1995-2009, chosen at random. The aim of the paper is to determine the clinical results of nasal septum operations in developmental age.
Material and methods. The study included children operated on for deviation of the nasal septum in the Paediatric Otorhinolaryngology Clinic of the Medical University of Warsaw during 1995-2009. The patients were evaluated on the basis of precise medical history, laryngological examination and anterior rhinomanometry.
Results. In the majority of patients we gained an improvement of the clinical picture.
Discussion. Our research indicates that results of septoplasty include proper nasal patency and general normal development of the treated child.
Conclusions. Septoplasty in children gives good clinical and laboratory results.
INTRODUCTION
Deviation of the nasal septum in children may be congenital or acquired. The most common cause of acquired deformations of the nasal skeleton are injuries. Other causes include congenital irregular growth of the facial skeleton and intrauterine injuries (1, 2, 3). Once it was thought that nose operations should be delayed until the end of the nose?s growth. It was thought that the operation might disturb further nose growth (2, 3). In the light of experience gained in the Paediatric Otorhinolaryngology Clinic of the Medical University of Warsaw and reports from world-leading research centres it transpires that nasal septum operations should be performed regardless of the age of the patient. Delay and toleration of impaired nose patency can have serious health effects due to the impact on the somatic and psychological development of the child (1, 2, 3, 5). Indications for nasal septum operation include the following: impairment of nasal breathing, frequent infections of upper airways, and ? as a relative indication ? pathological appearance of the nose. Basic differences between an adult patient and a child concern the nasal cartilage, which is more fragile and brittle in a child, and the mucoperiosteal flap, which is more enduring in a child.
Child nasal septum operations have to fulfil Cottle?s three basic rules:
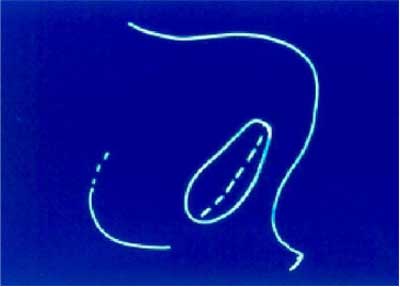
1. Mucous membrane cannot be cut; cutting half crosswise should be in the vestibule of the nose.
2. The operation should be carried out symmetrically.
3. Cartilaginous parts of the nasal septum cannot be resected; they can be moved. Resection, if it is necessary, may be applied only to the bony parts.
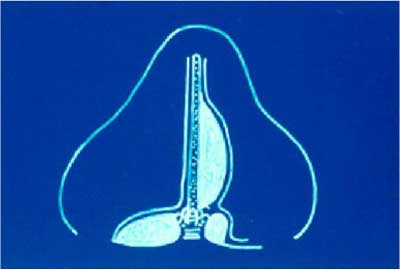
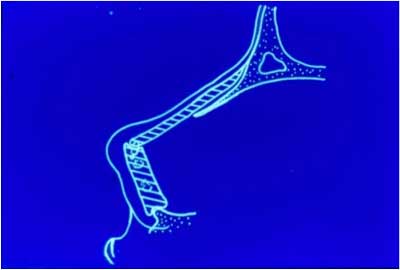
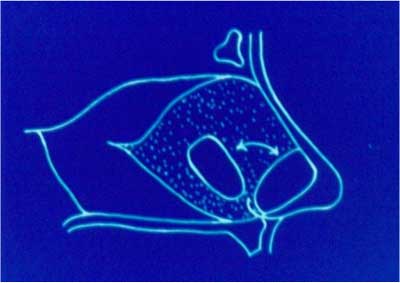
The operation starts with a half crosswise cut in the column area, then the front edge of the four-sided cartilage is located. The upper tunnels are made through the separation of the mucoperiosteal flaps, while making the front nose spine visible and separating the periosteum along the base of the nasal septum causes the creation of the lower tunnels. Connecting the tunnels causes the creation of the common nose tunnel. After defragmentation of the nasal septum cartilage, there follows the reimplantation with transposition (rotation of the cartilage) or translocation (far dislocation) if it is necessary and its positioning in the fibular position. The pouch is made in the column and the cartilage is fixed using the bridle sutures. The half crosswise cut is sutured, and the nasal septum is immobilized by means of Teflon plates with mattress sutures and tamponade of the nasal cavity.
Child nasal septum operation is a method implemented in clinical practice in the 1950s. Its performance in Poland started in 1979. So far, over 3000 such operations have been performed and analysed in the Paediatric Otorhinolaryngology Clinic of the Medical University of Warsaw.
Rhinomanometer measurements of nose patency have been made since 1978. The examined person is told to exhale through the nose. One of the nasal foramen is sealed and connected with the arm of the water manometer. The air is not flowing through this pipe so the pressure at all of its points is the same and corresponds to the pressure of the air in the posterior nares area. The second arm of the water manometer is connected with the inside of the mask, where the pressure is the same as in the anterior nares, so the manometer shows the difference in pressure between the anterior and posterior nares. During exhalation through the nose the flowmeter registers maximum air flow through the unsealed nasal foramen (7).
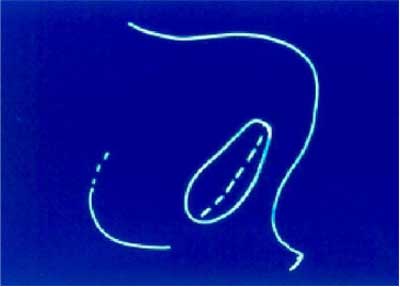
Fig. 1. Half crosswise cut.
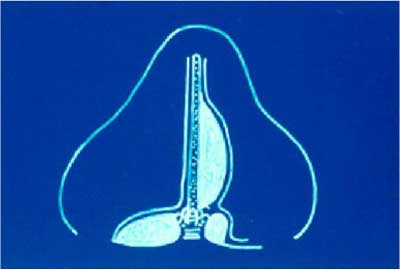
Fig. 2. Set of tunnels.
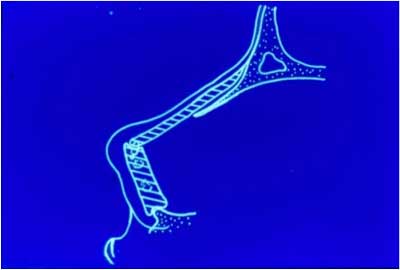
Fig. 3. Scheme of support of column and dorsum of nose.
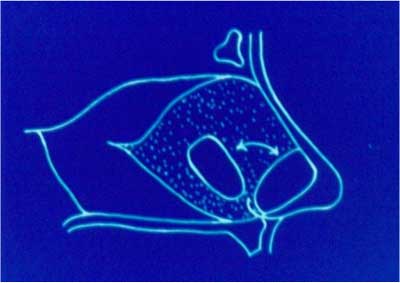
Fig. 4. Scheme of transposition and translocation.
AIM
To perform an analysis of patients operated on because of deviation of the nasal septum during 1995-2009, chosen at random. The aim of the paper is to determine clinical results of nasal septum operations in developmental age.
MATERIAL AND METHOD
725 children were examined (201 girls, 524 boys aged from 2 and 3/12 to 18 and 8/12) in whom an operation of the nasal septum was performed in the Paediatric Otorhinolaryngology Clinic of the Medical University of Warsaw during 1995-2009. The patients were evaluated on the basis of the precise medical history of ailments prior to the operation, the number of injuries prior to and after the operation, as well as the labour course. In laryngological examination the nose patency, appearance of the nose and the centre part of the face, as well as general development of the child, were evaluated. Anterior rhinomanometric measurements were carried out.
RESULTS
With regard to different dynamics of growth of nasal skeleton in adolescence we divided patients into 3 groups: I ? under 10; II ? 10-12; III ? over 12. Group I included 170 patients, group II 138 patients, and group III 417 patients. In the studied group in 34 cases osteotomies were performed, in 15 cases transplantation of preserved cartilage, and in 8 cases transplantation of autogenic cartilage. The numbers of procedures performed in particular groups are presented in table 1.
Table 1. The numbers of procedures performed in particular groups.
| Age group | Osteotomies | Transplantation of cartilage |
| preserved | autogenic |
| Under 10 | 6 | 7 | 2 |
| 10-12 | 9 | 2 | 1 |
| 12-18 | 19 | 6 | 5 |
According to the medical history taken before the surgical procedure nasal trauma occurred in 38 patients in the group under 10, in 41 in the group of age 10-12, and in 98 in the group over 12.
The longest period between an operation of deviated septum and follow-up examination was 13 years and 11 months and the shortest one was 1 year and 7 months. Post-operative follow-up was based on clinical examination and rhinomanometric examination. Fifty-six patients (7.7% of children operated on in this period in the Paediatric Otorhinolaryngology Clinic) applied for a follow-up examination. These results, according to the long period of observation and age of the patients, should be considered as an average.
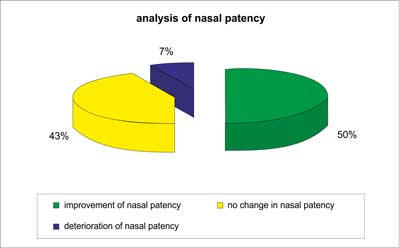
In the rhinomanometric examination the nasal patency and resistance produced by the skeleton of the nose were estimated. Rhinomanometric examinations were conducted only without decongestion of the mucosa of the nose and such ailments as allergy can have an influence on the results of rhinomanometry after surgical treatment. The rhinomanometry that was carried out prior to surgery was compared with the one carried out after the surgery. The results of rhinomanometry allowed estimation of the influence of septoplasty on nasal patency, and they are as follows:
? improvement of nasal patency 50% (28 patients),
? no change in nasal patency 42.8% (24 patients),
? deterioration of nasal patency 7.2% (4 patients),
In the group of 56 patients who underwent a follow-up rhinomanometry 7 children (12.5%) had significant nasal traumas after surgical treatment, which can influence the subjective and objective estimation of the result of the surgical procedure.
In the majority of patients we gained an improvement of the clinical status.
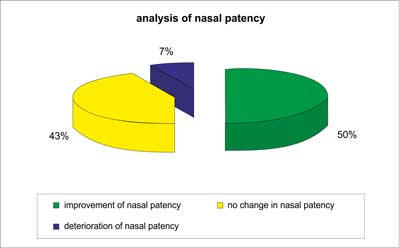
Diagram 1. Analysis of nasal patency.
DISCUSSION
Plastic surgery of deviated nasal septum in children engenders controversies, because of ambiguous indications for conducting this type of procedure and also because of difficulties in predicting the post-operative results in the constantly growing nose. Cooperation with a child demands more patience from the doctor as well as proper medical instruments (6). In this study active anterior rhinomanometry was used to estimate and compare pre- and post-operative results. This examination enables one to collect objective data (7). This study indicates that results of septoplasty include proper nasal patency and general normal development of the treated child. The operations were performed according to Cottle?s method, which does not have a negative influence on subsequent development of the treated nose (12, 16). When establishing indications for septoplasty in children one should take into consideration the degree of impairment of nasal patency, not the age of the patient (8). According to Emami the nasal septum in a patient who has undergone numerous traumas should be operated on as soon as possible in order to prevent the development of recurring infections of the upper respiratory tract, bronchitis or rhinosinusitis (9). The region of the column and of the dorsum of the nose plays an important role in children. Destruction of the nasal septum in the course of septal abscess or after a severe, extensive trauma is an indication for cartilage transplantation. Withdrawal from early reconstruction of deviated nasal septum can lead to disturbance of the growth of the nose (10, 11, 13, 14, 15).
Post-traumatic deviations of nasal septum appear more often in hyperactive children. Septoplasty improves function of the upper respiratory airways, but only to a lesser degree has an influence on motor activity of a child; therefore we can assume that nasal traumas after surgery will occur with a frequency comparable to the period before surgery. This fact can affect the long-term results. Operations according to Cottle?s method require continual monitoring and analysis of material. The presented study is only an extract and it is being continued with consideration of still developing surgical methods and possibilities.
CONCLUSIONS
1. In every case when deviated septum of the nose impedes breathing through the nose it should be treated operatively.
2. Septoplasty in children allows one to gain good clinical and laboratory results. Septoplasty according to Cottle permanently improves nasal patency, independently of age. It has a positive influence on the functioning of the whole respiratory tract.
3. No disturbance in the growth of the nose was observed.
4. Defect of cartilage of the septum can be replaced with a fragment of cartilage collected from a place with a similar growth potential.
5. Healing of the nose proceeded without complications and transplants were accepted.
Piśmiennictwo
1. Chmielik M: Schorzenia otorynolaryngologiczne u dzieci. (red.) M. Chmielik 2008; 81-82. 2. Chmielik LP, Chmielik M: Operacje nosa u dziecka. Magazyn Otolaryngologiczny, 2003 IX, suplement IV. 3. Bluestone CD et al.: Pediatric Otolaryngology. Fourth Edition, 2003; 2. 4. Chmielik M: Operacyjne leczenie zaburzeń drożności nosa u dzieci. Otolaryng Pol 2006; LX, 5: 675-685. 5. Pirsig W: Septal plasty in children: influence on nasal growth. Rhinology 1977; 15(4): 193-204. 6. Can IH et al.: Acoustic rhinometry in the objective evaluation of childhood septoplasties. Inter Jour of Ped Totrhinolar 69(2205): 445-448. 7. Chmielik M: Ocena spirograficzna i rynomanometryczne zmodyfikowanej techniki Cottle?a w operacjach przegrody nosa u dzieci ? praca habilitacyjna 1987. 8. Dispenza F et al.: Management of naso-septal deformity in childhood: Long-term results. Auris Nasus Larynx 2009; 36, 665-670. 9. Emami AJ, Brodsky L, Pizzuto M: Neonatal septoplasty: case report and review of the literature. Inter Jour of Ped Otorhinolar 1996; 35, 271-275. 10. Chmielik M, Zawadzka-Głos L, Wachulski B, Brożek E: Chrząstka konserwowana w operacjach rekonstrukcji nosa u dzieci. 40 lat bankowania i sterylizacji radiacyjnej tkanek w Polsce ? Przeszczep w walce z kalectwem 2003: 253-256. 11. Zawadzka-Głos L, Chmielik M, Wachulski B: Rekonstrukcja przegrody nosa u dzieci ? odległe wyniki. Nowa Pediatria 2005(3); 100-101. 12. Crysdale WS: Septoplasty in children ? yes, but do the right thing, Arch Otolaryngol Head Neck Surg 1999; 125(6): 701. 13. Béjar I et al.: Nasal growth after external septoplasty in children. Arch Otolaryngol Head Neck Surg 1996; 122(8): 816-21. 14. Healy GB: An approach to the nasal septum in children. Laryngoscope 1986; 96(11): 1239-42. 15. Derkay CS: A conservative role for septoplasty in young children. Arch Otolaryngol Head Neck Surg 1999; 125(6): 702-3. 16. Christophel JJ, Gross CW, Pediatric septoplasty. Otolaryngol Clin North Am 2009; 42(2): 287-94.