© Borgis - New Medicine 4/2010, s. 17-129
*Elżbieta Mazur
Acute pharyngotonsillitis:
current diagnosis and treatment**
Medical Microbiology Department, Medical University of Lublin
Head of the Department: prof. Maria Kozioł-Montewka MSc, PhD
Summary
Although its etiology is viral in about 80% of cases, antibiotics are frequently prescribed in the treatment of pharyngotonsillitis. Inappropriate use of antibiotics is a major cause of bacterial resistance, particularly among respiratory pathogens. Many countries all over the world, including Poland, have national guidelines for the diagnosis and treatment of respiratory tract infections to minimize unnecessary antibiotic prescriptions. This review paper presents current diagnosis and treatment of acute pharyngotonsillitis according to Polish Recommendations 2010.
Introduction
Acute pharyngotonsillitis is an illness that often leads patients to consult general practitioners, pediatricians, internists and ear, nose and throat specialists and results in a high degree of absence from daycare, school and work. It can be caused by a wide variety of pathogens. Viruses account for 70-85% of pharyngotonsillitis cases in children over 3 years of age and for 90-95% of cases in adults (1). Rhinoviruses, coronaviruses, adenoviruses, Coxsackie A, influenza, parainfluenza, RSV and herpes family viruses all may cause pharyngotonsillitis (1-4). Bacteria are responsible for 15-30% of pharyngotonsillitis cases in children and for 5-10% of cases in adults (1, 5). Among them, the most important one is Streptococcus pyogenes (Streptococcus beta-hemolytic group A, GAS). Beta-hemolytic streptococci belonging to other groups (predominantly C and G) are detected less frequently (1, 6-8). Other bacteria cause acute pharyngotonsillitis only sporadically (1, 5).
Although its etiology is viral in about 80% of cases, antibiotics are frequently prescribed in the treatment of pharyngotonsillitis (1, 5, 9). Inappropriate use of antibiotics is a major cause of bacterial resistance, particularly among respiratory pathogens (1, 5, 10, 11). Antibiotic consumption in Poland proved to be one of the highest in comparison with other European countries. Also, the percentage of Streptococcus pneumoniae strains resistant to penicillin is soaring (1, 5). Bacterial resistance is currently recognized as a global health problem. Many countries all over the world, including Poland, have national guidelines for the diagnosis and treatment of respiratory tract infections to minimize unnecessary antibiotic prescriptions. The national recommendations differ from each other because the epidemiological situation in different countries varies (1, 3, 5, 12, 13).
Patients with streptococcal pharyngotonsillitis should be treated with antibiotics to prevent rheumatic fever and local complications such as peritonsillar abscess, mastoiditis and sinusitis (1, 2, 14-16). However, it is of utmost importance to prevent prescription of antibiotics for pharyngotonsillitis which is viral in origin (1, 2, 14). Therefore, the differentiation between bacterial pharyngotonsillitis and that of viral etiology is crucial (3, 5).
Clinical differentiation of streptococcal and viral pharyngotonsillitis
In general, the clinical features of GAS pharyngotonsillitis are not specific and cannot be easily differentiated from those of viral origin; therefore a diagnosis based only on clinical grounds is impossible. Various clinical and epidemiological factors may indicate higher probability of streptococcal etiology, but the diagnosis must be confirmed by laboratory methods. Epidemiologically GAS pharyngotonsillitis is often seen in children between 5 and 15 years of age and tends to occur in colder months of the year. Patients with GAS pharyngitis often complain of pain while swallowing, fever, enlarged cervical lymph nodes and fatigue. Headache, nausea, vomiting and abdominal pain may be seen, particularly in children. Tonsils are reddened and swollen. The roof of the mouth may have fine petechial lesions. Although none of these are specific for GAS pharyngotonsillitis, absence of fever or presence of clinical features such as cough, hoarseness, conjunctivitis, runny nose, viral exanthem and diarrhea are common symptoms of viral upper respiratory tract infections (1, 2, 14, 17).
The basic aim of clinical differentiation is to evaluate the likelihood of streptococcal etiology. Depending on the result of clinical examination the decision is made about microbiological diagnostics and antibiotic therapy (if streptococcal pharyngotonsillitis is suspected) or about only symptomatic treatment and no further diagnostics (if the clinical picture suggests viral pharyngotonsillitis) (1, 3, 5, 17, 18). There are three clinical scales evaluating the probability of streptococcal pharyngitis: according to Breese, Centor?s with McIssac modification and Welsh?s. Since Breese?s scale does not allow streptococcal infection to be ruled out in patients with low risk and is based on the number of leukocytes in the blood, the other two are much more useful in everyday clinical practice. Walsh?s scale, however, has been verified only in adults. Therefore Polish Recommendations 2010 consider Centor/McIssac?s scale to be the most useful one, since it may be used for both children and adults (1, 5). Centor/
/McIssac?s scale, the likelihood of streptococcal infection and suggested management are depicted in tables 1 and 2.
Table 1. Centor/McIssac?s scale (adapted from Hryniewicz W. et al. (1) with permission).
| Criteria | Points |
| Temperature > 38°C | 1 |
| Absence of cough | 1 |
| Swollen, tender anterior cervical nodes | 1 |
| Tonsillar swelling or exudate | 1 |
| Age 3-14 years | 1 |
| Age 15-44 years | 0 |
| 45 years or older | -1 |
Table 2. Likelihood of streptococcal infection and suggested management (adapted from Hryniewicz W. et al. (1) with permission).
| Score | Percentage of patients with confirmed S. pyogenes infection | Suggested management |
| 0 | 2-3% | No further testing or antibiotic |
| 1 | 4-6% |
| 2 | 10-12% | Culture or RADT, antibiotics only if positive results |
| 3 | 27-28% |
| 4 | 38-63% | Treat empirically with antibiotics and perform culture or RADT, cease antibiotics if negative results |
Microbiological diagnosis of streptococcal
pharyngotonsillitis
In patients who have obtained 2 or more points according to Centor/McIssac?s scale a definitive diagnosis of GAS pharyngotonsillitis depends on the identification of the bacterium. Bacterial identification can be performed by throat swab culture or by rapid antigen detection test (RADT) (1, 2, 10, 14, 17, 19, 20). Success in isolating GAS in culture or getting a positive result using RADT depends on collection of a well taken throat swab. A sample must be obtained from both tonsils (or tonsillar fossae) and the posterior pharyngeal wall
(1, 2, 14, 17, 21). Inoculation of a throat swab onto blood agar remains the gold standard for diagnosis, with a sensitivity of 90-95% (1, 5, 18). A major disadvantage of throat culture is the delay (overnight or longer) in obtaining a result (4, 17). Although rapid tests are more expensive than culture, results are obtained faster, usually within 10-20 minutes (17, 22). Rapid antigen detection tests are now also highly specific (> 95%) and sensitive
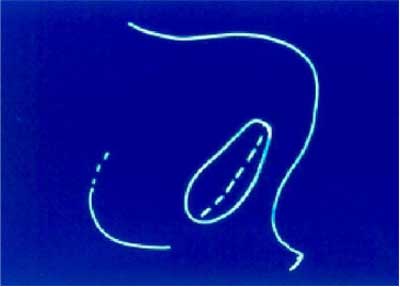
(70-90%) (1, 5, 18). The high specificity of RADT means that treatment can be initiated if the result is positive. However, a negative result does not exclude a diagnosis of GAS pharyngitis and should be confirmed by culture (1, 5, 20, 23). The algorithm for the diagnosis and treatment of acute pharyngotonsillitis is shown in figure 1.
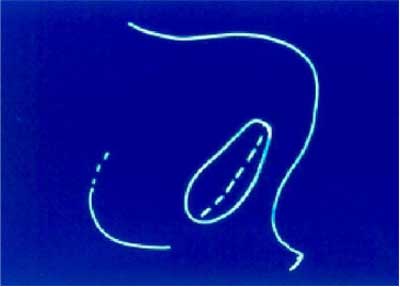
Fig. 1. Algorithm for the diagnosis and treatment of acute pharyngotonsillitis (adapted from Nascimento-Carvalho CM (11) with permission).
Antibiotic therapy in acute streptococcal
pharyngotonsillitis
According to American, Canadian and most European guidelines, including Polish Recommendations 2010, phenoxymethyl penicillin for 10 days is currently the antibiotic therapy of choice for GAS pharyngotonsillitis (1-5, 12, 13). Penicillin has stood the test of time satisfactorily since despite over 50 years of use, no penicillin-resistant GAS strains have so far been detected. Moreover, it has a narrow antimicrobial spectrum, low cost and an impressive safety profile (1, 2, 5, 12, 24). The only disadvantage is lack of compliance. However, this problem may be avoided by intramuscular injection of a single dose of benzathine penicillin G. Patients who are allergic to penicillin should be treated with first generation cephalosporin (cefadroxil). Only patients allergic to beta-lactam antibiotics should be treated with macrolides. However, the susceptibility of S. pyogenes to macrolides varies depending on the region and the level of consumption (1, 4, 5, 11). In 2008 about 11% of S. pyogenes strains isolated from patients with pharyngotonsillitis in Poland proved to be resistant to macrolides. Moreover, the predominant type of resistance to macrolides in our country is target modification due to ribosomal methylation, which means that such strains are simultaneously resistant to macrolides and lincosamides (1, 3, 5, 25). Since susceptibility of S. pyogenes to macrolides is unpredictable, treatment with these antibiotics must always be preceded by performing an antibiotic susceptibility test (1, 3-5). Besides, it has not been proved that macrolides prevent rheumatic fever (1, 5). According to the American Heart Association, the American Academy of Pediatrics, and the Infectious Diseases Society of America amoxicillin is now recommended as an alternative to penicillin (12). However, administration of amoxicillin in small doses, enough to treat acute pharyngotonsillitis, selects for S. pneumoniae strains resistant to penicillin. Therefore, amoxicillin is not recommended by Polish Recommendations 2010 (1, 3, 5).
It should be emphasized that antibiotic therapy may be delayed for several days and still achieve the goal of preventing rheumatic fever and spread of the disease (1, 3, 5, 12).
In summary, careful clinical examination of a patient with acute pharyngotonsillitis allows one only to suspect streptococcal etiology. Such suspicion should be confirmed by RADT or culture before making the decision about antibiotic therapy. Phenoxymethyl penicillin for 10 days is currently the antibiotic therapy of choice.
Following such a strategy we can minimize inappropriate use of antibiotics and prevent increasing bacterial resistance.
**The work was written under the auspices of the National Program on Antibiotic Protection.
Piśmiennictwo
1. Hryniewicz W et al.: Rekomendacje postępowania w pozaszpitalnych zakażeniach układu oddechowego 2010 (www.antybiotyki.edu.pl). 2. Stjernquist-Desatnik A, Orrling A: Pharyngotonsillitis. Periodontology 2000 2009; 49: 140-150. 3. Mazur E: Możliwości i ograniczenia diagnostyki mikrobiologicznej ostrych zapaleń górnych dróg oddechowych oraz budowanie podstaw racjonalnej antybiotykoterapii empirycznej na bazie danych lokalnych ? opinia mikrobiologa. Nowa Medycyna 2009; 2: 131-137. 4. Matas L et al.: Diagnóstico de las faringitis estreptocócicas. Enferm Infecc Microbiol Clin 2008; 26(Supl 13): 14-18. 5. Albrecht P, Radzikowski A: Optymalizacja antybiotykoterapii zakażeń dróg oddechowych w aspekcie programu ochrony antybiotyków. Nowa Medycyna 2009; 1: 13-20. 6. Fretzayas A et al.: The clinical pattern of group C streptococcal pharyngitis in children. J Infect Chemother 2009; 15: 228-232. 7. Tiemstra J, Miranda RLF: Role of non-group A streptococci in acute pharyngitis. J Am Board Fam Med 2009; 22: 663-669. 8. Lindboek M et al.: Clinical symptoms and signs in sore throat patients with large colony variant beta-haemolytic streptococci groups C and G versus group A. British Journal of General Practice 2005; 55: 615-619. 9. Moro ML et al.: ?Progetto bambini a antibiotici [ProBA]?: Why do paediatricians prescribe antibiotics? Result of an Italian regional project. BMC Pediatrics 2009; 9: 69 doi: 10.1186/1471-2431-9-69. 10. Al-Najjar FYA, Uduman SA: Clinical utility of a new rapid test for the detection of group A Streptococcus and discriminate use of antibiotics for bacterial pharyngitis in an outpatient setting. Int J Infect Dis 2008; 12: 308-311. 11. Nascimento-Carvalho CM: Outpatient antibiotic therapy as a predisposing factor for bacterial resistance: a rational approach to airway infections. J Pediatr (Rio J) 2006; 82(5 Suppl): S146-S152. 12. Baltimore RS: Re-evaluation of antibiotic treatment of streptococcal pharyngitis. Curr Opin Pediatr 2010; 22: 77-82. 13. Matthys J et al.: Differences among international pharyngitis guidelines: not just academic. Ann Fam Med 2007; 5: 436-443. 14. Brahmadathan KN, Gladstone P: Microbiological diagnosis of streptococcal pharyngitis: lacunae and their implications. Indian Journal of Medical Microbiology 2006; 24(2): 92-96. 15. Chazan B et al.: Clinical predictors of streptococcal pharyngitis in adults. IMAJ 2003; 5: 413-415. 16. Barash J: Group A streptococcal throat infection ? to treat or not to treat? Acta Paediatrica 2009; 98: 434-436. 17. Chopra H, Snyder JW: Laboratory diagnosis of streptococcal pharyngitis. University of Louisville School of Medicine Laboratory Advisor 2004; 2: 1-6. 18. Steer A, Danchin MH, Carapetis JR: Group A streptococcal infections in children. Journal of Paediatrics and Child Health 2007; 43: 203-213. 19. Tanz RR et al.: Performance of a rapid antigen-detection test and throat culture in community pediatric offices: implications for management of pharyngitis. Pediatrics 2009; 123: 437-444. 20. Fontes MJF et al.: Early diagnosis of streptococcal pharyngotonsillitis: assessment by latex agglutination test. J Pediatr (Rio J) 2007; 83(5): 465-470. 21. van der Veen EL et al.: Optimal site for throat culture: tonsillar surface versus posterior pharyngeal wall. Eur Arch Otorhinolaryngol 2006; 263: 750-753. 22. Llor C et al.: Association between use of rapid antigen detection tests and adherence to antibiotics in suspected streptococcal pharyngitis. Scandinavian Journal of Primary Health Care 2010; 28:12-17. 23. Hall MC et al.: Spectrum bias of a rapid antigen detection test for group A beta-hemolytic streptococcal pharyngitis in a pediatric population. Pediatrics 2004; 114: 182-186. 24. Shulman ST, Gerber MA: So what?s wrong with penicillin for strep throat? Pediatrics 2004; 113: 1816-1819. 25. Gracia M et al.: Antimicrobial susceptibility of Streptococcus pyogenes in Central, Eastern and Baltic European countries, 2005 to 2006: the cefditoren surveillance program. Diagn Microbiol Infect Dis 2009; 64: 52-56.